T cells attacking COVID-19 causing virus SARS-CoV-2 were found in uninfected controls suggesting that T cells can cross-react to the novel coronavirus, due to past infection from related coronavirus strains causing common cold.
‘The potential variation in T cell responses depending on severity to COVID-19 infection is key to understanding the role of how the immune system responds in the disease. This knowledge can also be used in vaccine design, evaluation and production.’
Read More..




Together, these new data address the poorly understood question of whether SARS-CoV-2-specific T cell responses vary in patients over time depending on disease severity, and helps to answer whether patients with more severe symptoms can generate protective virus-specific T cells at all. Read More..
The study also provides new clues regarding the cells responsible for excessive immune responses, including life-threatening "cytokine storms," and may also help inform vaccine design.
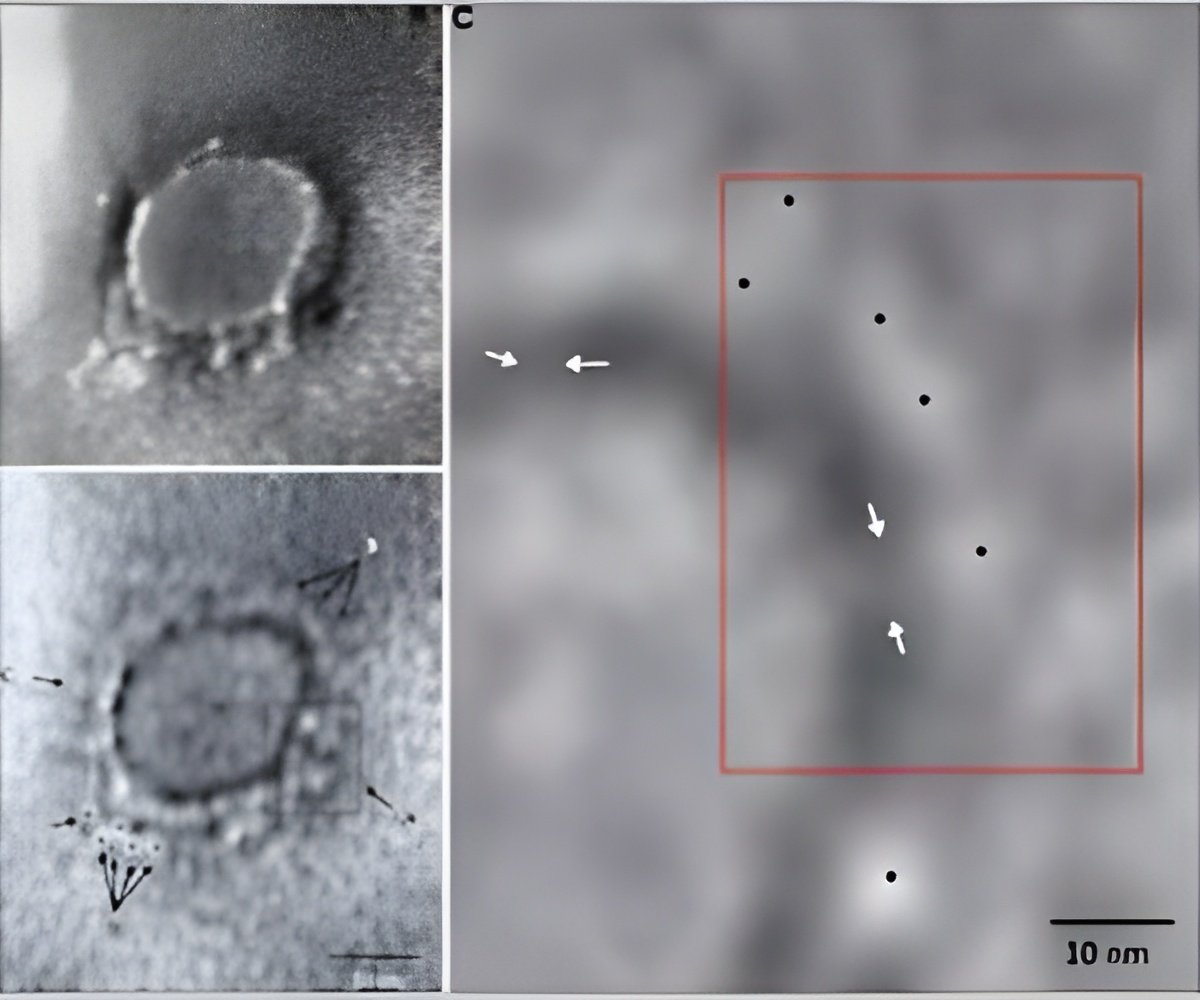
Daniela Weiskopf and colleagues extracted blood cells from 10 patients at weekly intervals starting soon after they were admitted to the ICU for COVID-19 and exposed these cells to "megapools" of known SARS-CoV-2 epitopes - a technique meant to capture a large fraction of total viral-reactive T cells. They found SARS-CoV-2-specific CD4+ helper T cells in all 10 patients and CD8+ "killer" T cells in 8 out of 10 patients, and characterized the cells' production of specific inflammation-triggering cytokines.
The strongest T cell responses were directed to the virus' spike (S) surface glycoprotein, supporting prior work that has pointed to the S protein as a promising target to induce virus-specific T cells. Furthermore, screening all patients at 0, 7, and 14 days after inclusion in the study revealed that SARS-CoV-2-specific T cells were present relatively early during the course of infection and increased in these patients over time.
Using the same T cell stimulation technique in age-matched healthy controls, the researchers found SARS-CoV-2-reactive T cells in 2 out of the 10 individuals.
Advertisement
Source-Eurekalert