COVID-19 may raise risks of blood-fat disorders, affecting cholesterol and heart health.
A six-year study in a real-world population reveals an increased incidence of dyslipidemia during COVID-19
Go to source)
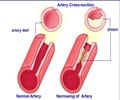
What is Dyslipidemia
Dyslipidemia is a condition marked by abnormal levels of lipids, like cholesterol and triglycerides, in the blood. This imbalance can lead to a higher risk of cardiovascular disease, as excess lipids may cause plaque buildup in the arteries, narrowing them and impeding blood flow. Often tied to lifestyle factors, genetics, or underlying health issues like diabetes, dyslipidemia may not present symptoms initially, making regular health screenings crucial. Treatment typically involves lifestyle changes, such as a balanced diet and regular exercise, and sometimes medication to help regulate lipid levels and reduce cardiovascular risks.‘#COVID-19 linked to a 29% increased risk of #dyslipidemia, a condition associated with #heartdisease and stroke. #cholesterol’





“Given the extent of the pandemic, this increase in dyslipidemia risk is a cause for concern around the world,” said study leader Gaetano Santulli, M.D., Ph.D., associate professor of medicine and of molecular pharmacology at Einstein. “Based on our findings, we would advise people to have their lipid levels monitored regularly and to consult with their healthcare providers about ways to treat dyslipidemia if detected, especially elderly individuals and patients with diabetes.” He noted that this advice would apply to all adults, not just those formally diagnosed with COVID-19, considering that many people have been infected without realizing it. To put these findings into context, it has been estimated that 53% of U.S. adults had dyslipidemia before the pandemic; a 29% increase in dyslipidemia incidence due to COVID-19 would mean that 68% of Americans may now be at risk for having lipid abnormalities.
In two previous studies, Dr. Santulli and his team found that COVID-19 raised the incidence of new cases of hypertension and type 2 diabetes. “In those analyses, we demonstrated that the risk of developing these disorders was still high three years after the pandemic; moreover, we noticed a suspicious increase in total cholesterol levels, which warranted a closer look,” said Dr. Santulli. In the new study, the researchers first determined the incidence of dyslipidemia in a group of more than 200,000 adults living in Naples, Italy, during the three years prior to the start of the pandemic (2017-2019). They then assessed the incidence of dyslipidemia in the same group during the three-year COVID-19 period (2020-2022), excluding from the analysis those people earlier diagnosed with dyslipidemia or who had previously been taking lipid-lowering medications.
The increase was even higher among people over age 65 and those with chronic conditions, particularly diabetes and obesity, cardiovascular disease, chronic obstructive pulmonary disease, and hypertension. The findings are the most definitive to date because other studies—most of them linking COVID-19 with modestly increased risks for blood-lipid problems—used as control groups different populations or people thought to have gone through the pandemic without becoming infected. However, significant numbers of people classified as “COVID-free” actually developed the disease but were either never tested or didn’t seek medical care.
“Our study did not attempt to determine whether participants had tested positive for COVID-19,” Dr. Santulli said. “Instead, because we had been following this group for many years prior to the pandemic, we were able to measure COVID’s overall impact on the population by simply comparing levels of dyslipidemia in the same group before and after the pandemic. Any increase in dyslipidemia incidence would almost certainly have to be the result of COVID-19.”
Advertisement
A separate study found that COVID-19 is a powerful risk factor for heart attacks and strokes for as long as nearly three years after an infection. “This investigation, published online a month after ours, essentially confirms our observations in this study, since dyslipidemia is a major contributor to cardiovascular disease,” said Dr. Santulli. “It also suggests that tackling dyslipidemia should reduce the risk of cardiovascular disease in those who have had COVID.” The researchers are now studying the effects of COVID-19 on cardiovascular-kidney-metabolic (CKM) syndrome, a recently described condition involving four connected medical problems—heart disease, kidney disease, diabetes, and obesity—all of which involve endothelial dysfunction.
Advertisement
- A six-year study in a real-world population reveals an increased incidence of dyslipidemia during COVID-19 - (https://www.jci.org/articles/view/183777)