CRISPR gene therapy trial for sickle cell disease offers hope by targeting the genetic cause directly.
CRISPR-SCD
Go to source) at UCSF Benioff Children's Hospital Oakland aims to cure sickle cell disease using non-viral CRISPR-Cas9 gene editing, a first-of-its-kind approach in the U.S. The research involves taking the patient’s blood stem cells to correct the mutation and returning those edited cells to the patient through a bone marrow transplant. It’s hoped the corrected blood stem cells will then multiply and create a new blood system, one free of sickle cell.
‘A revolutionary step in treating #sickle_cell_disease! #CRISPR gene editing is being used to directly fix the underlying genetic mutation. #gene_therapy’





“This therapy is intended to eliminate sickle cell disease by applying CRISPR technology that is safer than a standard stem cell transplant from a healthy bone marrow donor,” Mark Walters, MD, a professor of pediatrics at UCSF and principal investigator of the clinical trial and gene editing project. “It is a potential game changer for young sickle cell patients because the therapy eliminates the need for a suitable donor and removes the mutation for a life free of sickle cell disease.” Researchers are recruiting patients for treatment in California, beginning with up to six adults with sickle cell disease. A safety evaluation will be performed after the first three adult patients receive the treatment. If found to be safe and effective, it will expand to enroll three adolescents aged 12 to 17 years old. The trial is expected to last two years, with patients ideally being followed up for up to 15 years.
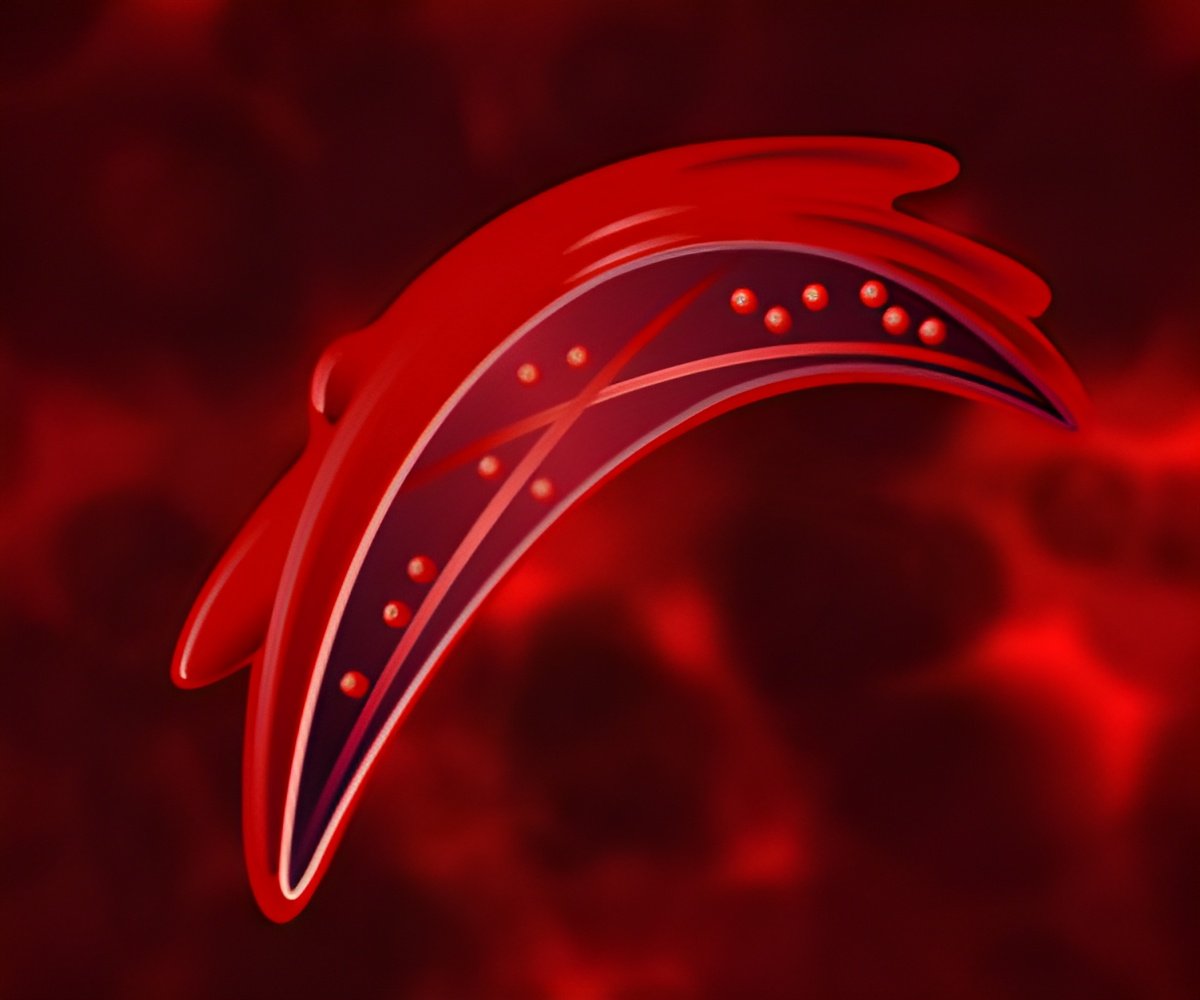
What is Sickle Cell Disease
Sickle cell disease is a genetic blood disorder caused by a single mutation in both copies of a gene coding for beta-globin. Beta-globin forms half of the oxygen-carrying molecule hemoglobin. This mutation causes hemoglobin molecules to stick together, deforming red blood cells into a characteristic “sickle” shape. These misshapen cells get stuck in blood vessels, causing blockages, anemia, pain, organ failure, and a significantly shortened lifespan. Sickle cell disease affects approximately 100,000 Americans and millions worldwide, with a disproportionate effect on the Black community.The project team from UCSF, the Innovative Genomics Institute (IGI) and UCLA have developed CRISPR_SCD001, a patient-specific blood stem cell therapy product derived from the patient that has been modified by a CRISPR-Cas9 nuclease to stimulate repair of the sickle mutation.
In the current trial, the patient’s blood stem cells will be extracted and sent to UCLA’s Human Gene and Cell Therapy Facility to be processed using electrical pulses that create temporary pores in their membranes. These pores allow the non-viral CRISPR-Cas9 platform to enter the cells and travel to the nucleus, where it corrects the sickle cell mutation before the cells are returned to the patient in a bone marrow transplant procedure.
Advertisement
The trial is part of a UC research consortium led by UCSF with UCLA and UC Berkeley. It will combine CRISPR technology developed at IGI – a joint UC Berkeley-UCSF initiative founded by Nobel Laureate Jennifer Doudna – with UCLA’s expertise in genetic analysis and cell manufacturing, as well as its clinical excellence in the field, and nearly 50 years of expertise at Benioff Children’s Oakland in sickle cell care, including cord blood and marrow transplantation, and gene therapy.
Advertisement
Reference:
- CRISPR-SCD - (https://curesickle.org/crispr-scd)