University of Illinois Health surgeons removed about six feet of small intestine from 59-year-old Bruce Lugo and transplanted the segment into his daughter.

‘Living-donor small intestine transplants - in which a portion of the organ is taken from a compatible donor - have outcomes comparable to cadaveric transplants.’





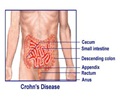
Living-donor small intestine transplants - in which a portion of the organ is taken from a compatible donor, usually a close family member - have outcomes comparable to cadaveric transplants. However, receiving an organ from a relative bypasses the wait on a list for a cadaveric organ that is a good match. Lugo was a sophomore in high school and just 16 years old when she experienced ongoing severe pain in her abdomen that brought her to a local hospital. "I wasn't feeling well enough to go to school, but it took a while to find out what was causing the pain," she said. X-ray and MRI scans ultimately identified a benign mass behind her stomach the size of a golf ball.
She underwent surgery at another hospital to remove the mass, but a complication caused her entire small bowel to gradually die off, and additional surgeries were required to remove it. Since then, Lugo has lived with virtually no small intestine. Surgeons connected a short, remaining section of her small intestine near her stomach directly to her large intestine. Because the small intestine's primary function is to absorb nutrients from food, Lugo required total parenteral nutrition, or TPN, in which nutrition is delivered intravenously.
"Bloodstream infections that originate in the intravenous line and clotting of the handful of veins we use to place the feeding line are some of the life-threatening risks associated with TPN," said Dr. Enrico Benedetti, chief of transplant surgery at UI Health, who led the surgical team. "The presence of these life-threatening complications is the main indication for considering a small bowel transplant, which allows freedom from TPN when successful."
After waiting on the transplant list for three years at another center, Lugo was referred to UI Health in the fall to be evaluated for a living-donor transplant. At that time, she was experiencing recurrent line infections and three of the six veins used for TPN had collapsed.
Advertisement
Source-Newswise