Video-based decision aids lead to lower rates of knee and hip replacement surgeries, say researchers.
This is the first time anyone has explored how using decision aids in routine practice can affect health care and costs, Dr. Arterburn said. It is also the first major study of decision aids for knee and hip replacement.
"Our study's real-world findings with the orthopedic decision aids are consistent with results of prior randomized trials of other kinds of decision aids," Dr. Arterburn said. Those trials found that people were more likely to make informed choices that aligned with their preferences when they had access to objective, easily understood, evidenced-based information about the risks and benefits of treatment options. They also tended to choose more conservative, less invasive options—and to be more satisfied with whatever happened, regardless of whether they chose a surgical intervention.
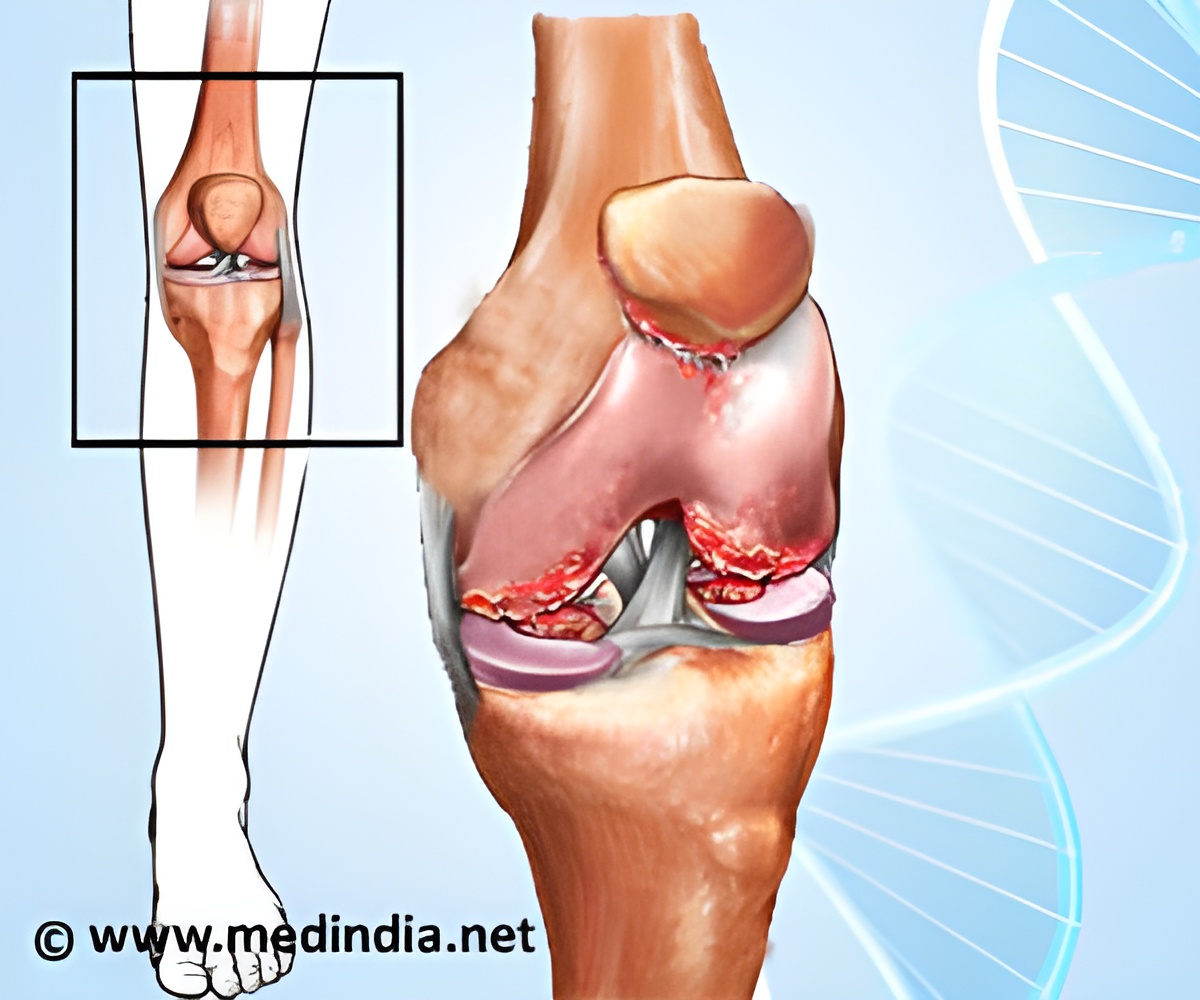
The findings are important because more than 27 million Americans have osteoarthritis, which can cause severe pain and restrict functioning, including employment, Dr. Arterburn said. Joint replacement is among the most common U.S. orthopedic procedures, with more than 650,000 knees and 250,000 hips replaced each year, at a combined cost of $15.6 billion.
"Joint replacement can reduce pain and improve function for many patients," said co-author Charles F. Jung, MD, Group Health's chief of orthopedics. "But so can many nonsurgical actions that people can take to help ease their knee and hip arthritis." Dr. Jung said. Because excess weight strains joints (particularly knees), the main action is to lose any extra weight. Other examples are physical therapy, nonsteroidal anti-inflammatory drugs like ibuprofen, avoiding injury, and mixing up a variety of low-impact activities, like walking, swimming, and biking. "These are the same things that we suggest for patients who choose surgery, to lower the risk of their new joint failing and needing to be replaced again, which can be more complicated," he added.
"People often have wishful thinking about what joint replacement can do for them," Dr. Jung said, "like our patient who thought he'd be his club's singles-tennis champ again." Biased information sources, including direct-to-consumer ads for artificial joints, may fuel such expectations. By contrast, decision aids serve as a balanced reality check, describing factors including the three-month recovery time, the 10- to 20-year lifespan of artificial joints, and risks such as infection and possible reoperation. "After people see a decision aid, they tend to come into our office with more realistic expectations, and we can have a more focused discussion about what matters most to them as individuals," he added.
Advertisement
"In 2009, as part of a large-scale quality-improvement program, we started introducing decision aids for all our patients facing decisions about these elective surgeries," said co-author Matthew Handley, MD, Group Health's associate medical director for quality and informatics. Group Health leaders were already convinced by the existing evidence that introducing decision aids would be good for patients. "So instead of just repeating another randomized trial, we started incorporating the decision aids into care for everyone," he added.
Advertisement
Tracking nationwide Medicare spending for more than two decades, Dartmouth Atlas of Health Care experts call care for clinical gray areas "preference-sensitive," because it should reflect what individual patients need and prefer. But instead, they have found, this kind of care too often varies widely by geographical area, depending most on what local providers happen to want to do. Decision aids are meant to decrease these "unwarranted variations in care" by informing patients about the risks and benefits of treatment options. The aids may also help patients to clarify what they want and need, so their values and preferences carry more weight in the decision-making process.
In 2007, Washington became the first state to pass legislation recognizing the use of patient decision aids and "shared decision making" as a higher standard of informed consent. In shared decision making, health care providers inform patients about their options—often using decision aids—and help them to clarify what matters most to them and to make an informed decision.
Most of the September issue of Health Affairs focuses on payment reform: moving away from fee-for-service payment, where providers earn more for giving patients more tests and treatments, as in most of U.S. health care now. This concerns many people because, like getting less health care than needed, getting too much care—overdiagnosis and overtreatment—can harm patients. Payment reform is one solution that has been proposed for decreasing unwarranted variations in care. At Group Health, health care providers are paid a salary and receive no bonus for doing more procedures. So financial incentives at Group Health are aligned to keep patients healthy, instead of giving them more tests and treatments.
"But implementing decision aids and shared decision making can work well in fee-for-service settings too," Dr. Arterburn said. "They just need health care providers who are concerned about having their patients make high-quality informed decisions—and most providers are."
Source-Eurekalert