Researchers have found that opting for a decompression surgery could be an effective way of treating cervical spondylotic myelopathy (CSM).
The study, "Efficacy and Safety of Surgical Decompression in Patients with Cervical Spondylotic Myelopathy: Results of the AOSpine North America Prospective Multi-Center Study," published in the Journal of Bone and Joint Surgery, found that patients with mild, moderate and severe CSM show significant recovery after undergoing decompression surgery – a procedure that alleviates pressure on the nerves of the spinal cord.
"The results of this trial support the use of decompression surgery as a viable treatment for Cervical Spondylotic Myelopathy and could lead to a change in practice to treat this condition," said Dr. Michael Fehlings, neurosurgeon and Medical Director of the Krembil Neuroscience Centre, Toronto Western Hospital and the study's lead author. "With few existing interventions available for these patients, it is encouraging to have data showing improvements in quality of life as a result of surgery, in some cases, even reversing serious neurological damage that could have resulted in paralysis."
To date, the limited research and mixed reports have concluded that there was no added benefit from surgical intervention for CSM patients, and that the best approach was to monitor the progression of their condition and, in some cases, treat conservatively with non-surgical approaches. However, in 30 to 50 per cent of CSM cases, it has been observed that the condition gets progressively worse, impairing patients' ability to walk and perform daily tasks such as dressing themselves and performing their own personal hygiene. This study clearly shows that many more patients with CSM could benefit from surgery than previously thought.
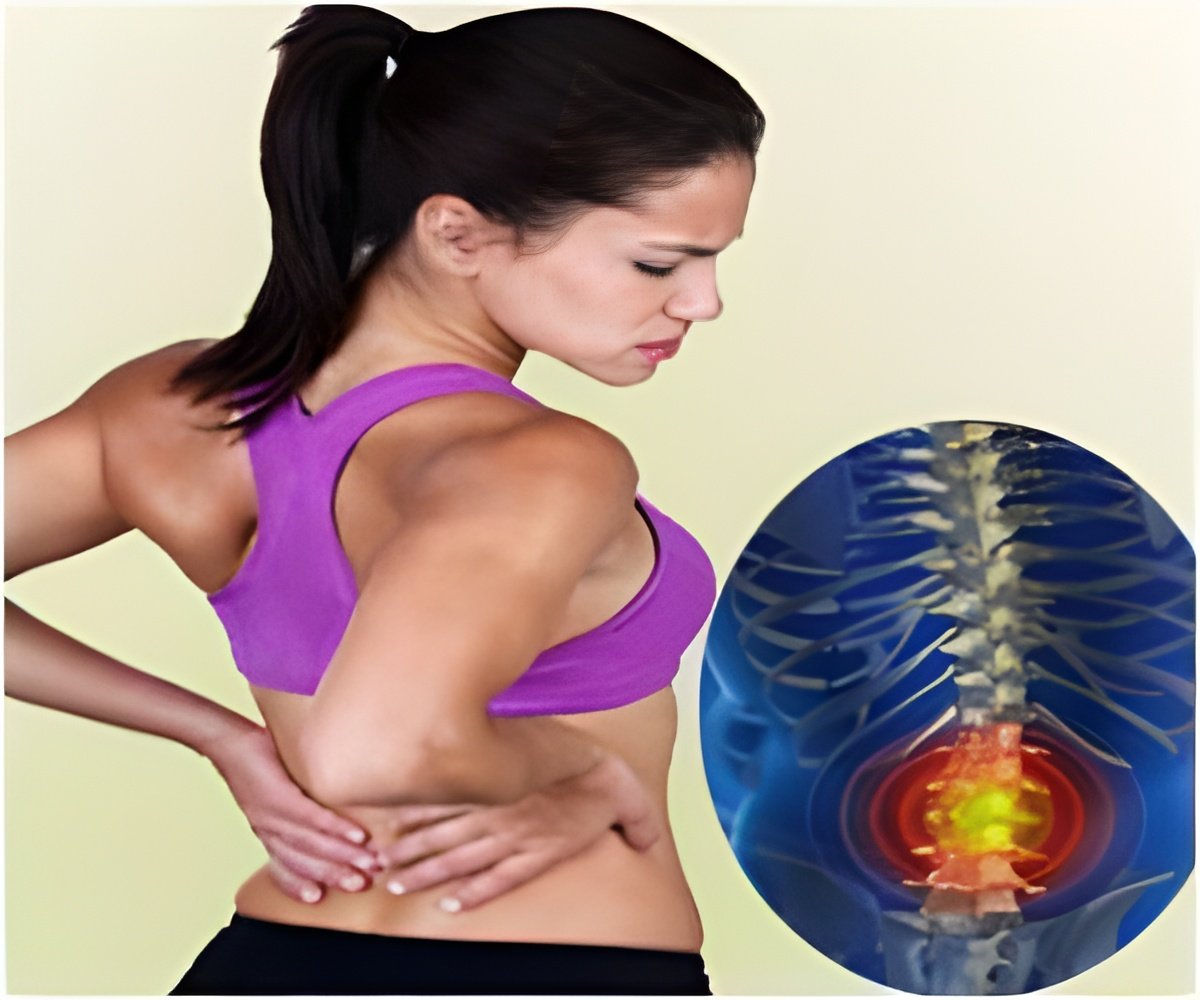
CSM is the leading cause of spinal cord dysfunction in the world, mostly affects people over the age of 50 and is very common in people of Asian and South Asian descent. Over time, the normal process of aging can sometimes lead to the narrowing of the spinal canal creating pressure on the spinal cord. As CSM progresses, it can cause neck stiffness, arm pain, numbness in the hands and, in severe cases, inhibits movement in limbs, impairs walking and can eventually lead to paralysis.
An unrecognized condition that is often misdiagnosed, CSM incidence and prevalence remain undetermined in Canada but, based on clinical caseloads and statistics from the U.S., is estimated to occur among 20 per cent of Canadians with approximately 10 per cent of them requiring surgery to treat the spinal cord dysfunction.
Advertisement
From 2005 to 2007, researchers at 12 trial centres across North America, including Toronto Western Hospital, recruited patients with symptoms of CSM whose x-rays showed evidence of spinal cord compression. Patients were then categorized as having mild, moderate or severe CSM. The aim of the study was to evaluate the impact of decompression surgery on functional, quality of life and disability outcomes one year after patients had undergone surgery. The study also set out to determine, if the degree of improvement depended on the severity of CSM in patients before surgery.
Advertisement
At the one year follow up after decompression surgery, researchers found that the majority of study participants experienced statistically significant improvements in their condition. They also noted that for functional, disability and quality of life measures, the degree of improvement did not depend on the severity of preoperative symptoms, indicating that even cases of mild and moderate CSM benefit from surgical intervention.
"Although all patients experienced improvement in their condition after surgery, the challenge now is to ensure patients suffering from CSM receive surgical intervention in the earlier stages of the disease," Fehlings said. "This approach ensures patients avoid permanent neurological impairment, and will reduce costs to the healthcare system over the long term."
In light of the lack of existing information to treat CSM, researchers also used the data collected from the 278 patients participating in the trial to establish a prediction model of surgical outcomes in CSM patients. Also published today in the Journal of Bone and Joint Surgery, the accompanying paper "A Clinical Prediction Model to Determine Outcomes in Patients with Cervical Spondylotic Myelopathy Undergoing Surgical Treatment," will help clinicians determine which patients would benefit most from decompression surgery to treat CSM.
The first study of its kind to look at symptomatic CSM patients in order to determine surgical outcome, researchers analyzed the trial data to find the best combination of clinical and imaging factors to design a clinical outcome model that helps predict surgical results. The degree of surgical success in patients was measured by using the modified Japanese Orthopaedic Association score (mJOA), a widely accepted 18 point scale to assess functionality in patients with CSM. At the one-year follow up, a successful outcome from surgery was defined by a mJOA score equal or greater to 16, with patients scoring less than 16 perceived to have a failed outcome. The score of 16 – 18 is clinically accepted as indicating mild impairment.
The analysis determined that the presence of the following factors contribute to a negative outcome from surgery: smoking, older age, the level of severity of the spinal cord compression before surgery, the duration of CSM related symptoms, the dimensions of the affected area of the spinal cord, the presence of emotional or psychological symptoms such as depression and whether or not a patient's walking gait was impaired.
"CSM is the most common cause of spinal cord impairment and when misdiagnosed allows for the disease to progress," said Fehlings. "These studies support not only recommending surgery to treat CSM, but also provide guidelines of when to perform surgery and what patient criteria are more likely to lead to a full recovery."
Complications from surgery experienced by trial participants were brief and expected, with any persistent side effects occurring in 1 per cent or less of patients. Future research will help determine which decompression surgery technique has the best outcome for this procedure.
Source-Eurekalert









