Targeted magnetic resonance/ultrasound fusion biopsy was associated with increased detection of high-risk prostate cancer, compared to standard biopsy technique.
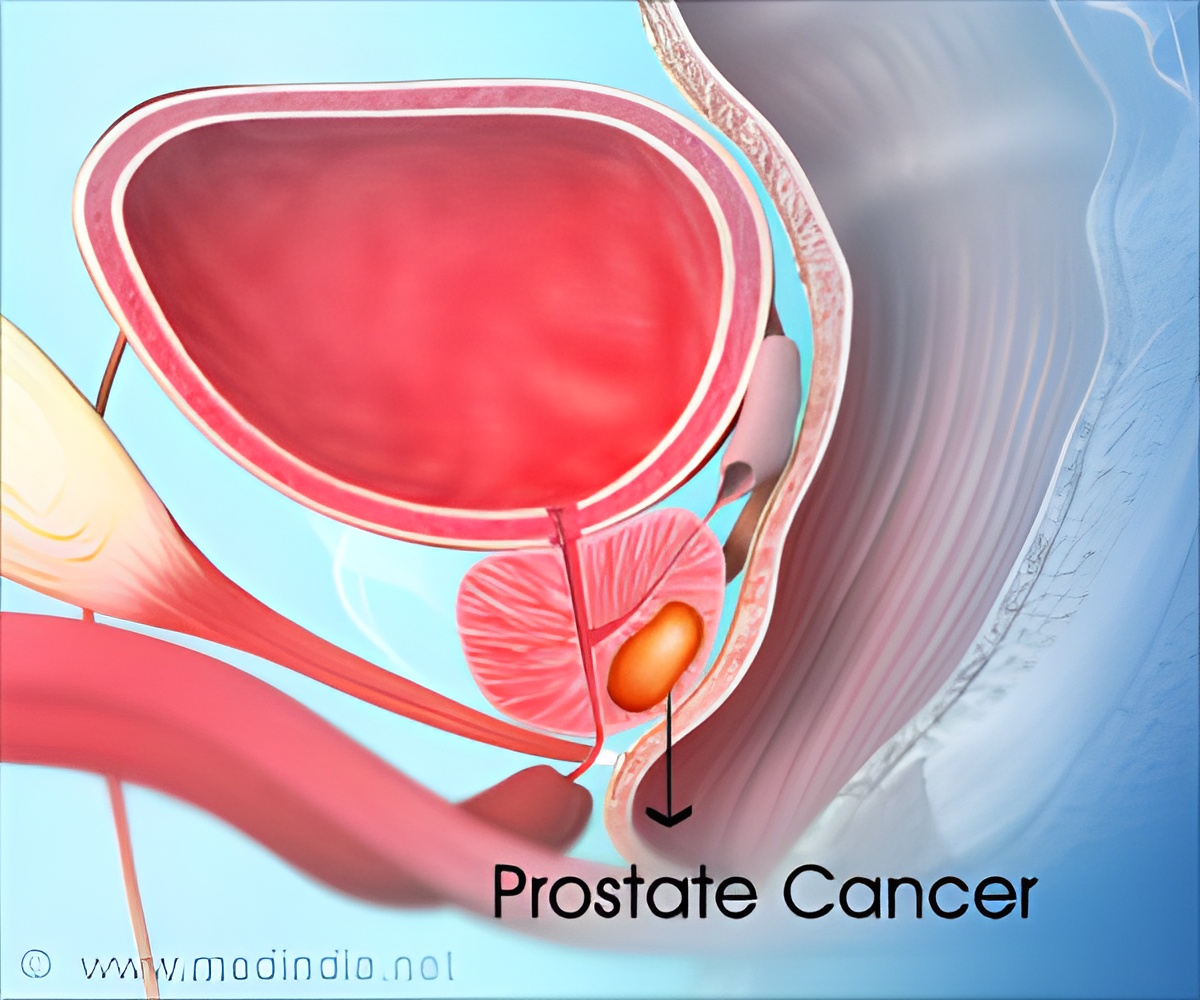
Peter A. Pinto, M.D., and M. Minhaj Siddiqui, M.D., of the National Cancer Institute, National Institutes of Health, Bethesda, Md., and colleagues examined the outcomes of 1,003 men who underwent an imaging procedure to identify regions of prostate cancer suspicion followed by targeted biopsy and concurrent standard biopsy from 2007 through 2014 at the National Cancer Institute. Patients were referred for elevated level of prostate-specific antigen (PSA) or abnormal digital rectal examination results, often with prior negative biopsy results.
Targeted biopsy diagnosed a similar number of cancer cases (461 patients) to standard biopsy (469 patients). There was exact agreement between targeted and standard biopsy in 690 men (69 percent) undergoing biopsy. However, the 2 approaches differed in that targeted biopsy diagnosed 30 percent more high-risk cancers vs standard biopsy (173 vs 122 cases) and 17 percent fewer low-risk cancers (213 vs 258 cases).
Adding standard biopsy to targeted biopsy lead to 103 more cases of cancer (22 percent); however, of these, 83 percent were low risk while only 5 percent were high risk; 12 percent were intermediate risk. Thus, the usefulness of combining these methods was found to be limited, with the number needed to biopsy by standard biopsy in addition to targeted biopsy to diagnose 1 additional high-risk tumor was 200 men.
The predictive ability of targeted biopsy for differentiating low-risk from intermediate- and high-risk disease in 170 men with whole-gland pathology after prostatectomy (surgical removal of the prostate gland) was greater than that of standard biopsy or the 2 approaches combined.
"This study demonstrated that targeted biopsy could significantly change the distribution of risk in men newly diagnosed with prostate cancer toward diagnosis of more high-risk disease. Although these improvements in risk stratification could translate into substantial clinical benefits, it is important to recognize that this study is preliminary with regard to clinical end points such as recurrence of disease and prostate cancer-specific mortality. These findings provide a strong rationale for the conduct of randomized clinical trials to determine the effect of targeted biopsy on clinical outcomes," the authors write.
(doi:10.1001/jama.2014.17942; Available pre-embargo to the media at http://media.jamanetwork.com)
Advertisement
"Decisions to adopt new technologies such as this one that occupy a largely unregulated space ultimately rely on clinicians and payers, based on available data," write Lawrence H. Schwartz, M.D., of the Columbia University College of Physicians and Surgeons, New York, and Ethan Basch, M.D., of the University of North Carolina, Chapel Hill, and Associate Editor, JAMA, in an accompanying editorial.
Advertisement
(doi:10.1001/jama.2014.17943; Available pre-embargo to the media at http://media.jamanetwork.com)
Editor's Note: Please see the article for additional information, including financial disclosures, funding and support, etc.
Source-Newswise








![Prostate Specific Antigen [PSA] Prostate Specific Antigen [PSA]](https://www.medindia.net/images/common/patientinfo/120_100/prostate-specific-antigen.jpg)