Most patients who received the Charcot's foot surgery remained infection-free and were able to walk normally.
‘173 of the 223 feet had good or excellent outcomes, which meant that they were free of ulcers and infections and able to walk outside the home using therapeutic footwear and custom foot braces.’





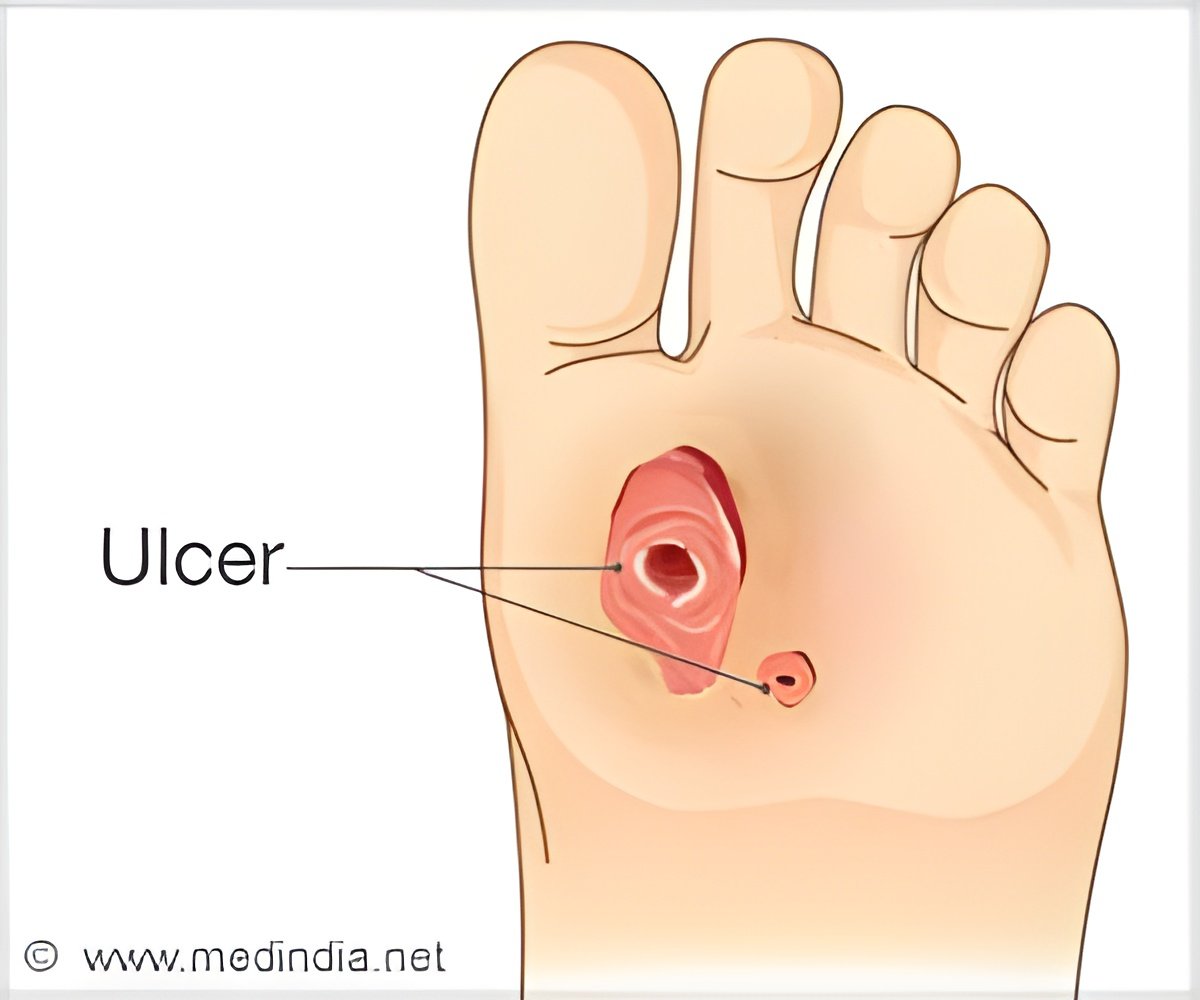
The growing number of diabetics, combined with the obesity epidemic, is increasing the incidence of Charcot foot. The condition typically occurs in diabetics who have neuropathy (nerve damage), which impairs the ability to feel foot pain. Charcot foot usually develops following a minor injury, such as a sprain or stress fracture. Because the patient doesn’t feel the injury, he or she continues to walk, making the injury worse. This can cause a deformity, or malposition of the foot, which eventually can lead to ulcers and infections of the bone. "Charcot foot is a debilitating condition that is very challenging to treat," Dr. Pinzur said. "But with the proper surgical treatment, most patients will be able to walk normally again."
Loyola Medicine has one of the leading programs in the country for treating Charcot foot, also called diabetic foot or Charcot arthropathy. Loyola takes an integrated approach, combining the expertise of orthopaedic surgeons, podiatrists, endocrinologists and other specialists.
Most patients can be treated successfully by immobilizing the foot. But a small percentage of patients, such as those in the Loyola study, develop severe deformities or bone infections.
Traditionally, a successful treatment for a severe case of Charcot foot was defined as clearing up the infection and preventing a foot amputation. The Loyola study used a stricter standard: in addition to resolving the infection and saving the foot, the patient had to be able to walk outside the home with the use of commercially available therapeutic footwear. Using this higher standard, 77.6 percent of the feet had favorable outcomes following surgery.
Advertisement
Seven patients died of unrelated causes within a year of surgery and 15 underwent partial- or whole-foot amputations.
Advertisement
A common treatment for severe Charcot foot is to put the patient in a cast. But bones can heal in deformed positions. It also is difficult or impossible for obese patients to walk on one leg when the other leg is in a cast. Patients typically have to use wheelchairs for as long as nine months, and after the cast comes off, they must wear a cumbersome leg brace.
However, traditional surgical techniques, in which bones are held in place by internal plates and screws, also are challenging. Bones already weakened by complications of Charcot foot could collapse under the patient’s weight.
Dr. Pinzur employs a technique that secures bones with an external frame, made of stainless steel and aircraft-grade aluminium. The device, called an Ilizarov circular external fixator, contains three rings that surround the foot and lower calf. The rings have stainless-steel pins that extend to the foot and secure the bones after surgery.
Following surgery, the device remains on the patient for 10 to 12 weeks. During that time, patients often are able to walk or at least bear some weight. After the fixation device is removed, the patient wears a walking cast for four to six weeks. The patient then progresses to a removable boot and finally to diabetic shoes.
Source-Eurekalert