More than 300,000 service members were diagnosed with mild traumatic brain injury MTBI between 2000 and 2015 in the United States.

‘A type of MRI called diffusion tensor imaging can help predict the long term effects for veterans who have sustained mild traumatic brain injury.
’





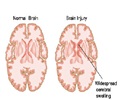
Current assessment of MTBI remains challenging due to the difficulties in establishing the diagnosis, predicting outcomes and separating the effects of MTBI from other conditions like post-traumatic stress disorder (PTSD). DTI uses measurements of water movement in the brain to detect abnormalities, particularly in white matter. Previous studies have linked DTI metrics to neurocognitive function and short-term functional outcomes in groups of patients. The desire to uncover possible long-term effects spurred Jeffrey B. Ware, M.D., from the Philadelphia VA Medical Center in Philadelphia, Pa., to evaluate combat veterans using this technique.
Dr. Ware and colleagues used brain MRI and DTI to study 57 military veterans who had a clinical diagnosis of MTBI upon return from deployment. The average length of time between injury and post-deployment evaluation was 3.8 years with an average follow-up duration of 1.4 years.
"All conventional MR images were interpreted as normal," Dr. Ware said. "We retrospectively analyzed the data from the DTI sequence to derive measures of white matter integrity, which we compared to clinical measures and subsequent outcome measures 6 months to 2.5 years after the initial evaluation."
The results showed significant associations between initial post-deployment DTI measurements and neurobehavioral symptoms, timing of injury, and subsequent functional outcomes. The measurements also correlated with greater healthcare utilization among veterans with MTBI.
Advertisement
"Our findings suggest that differences in white matter microstructure may partially account for the variance in functional outcomes among this population. In particular, loss of white matter integrity has a direct, measurable effect," Dr. Ware said. "It was illuminating to see the association between measures of white matter integrity and important outcomes occurring months to years down the road in our study population."
Advertisement
Source-Eurekalert