Digital versions of a standard molecular biology tool to detect a common tumor-associated mutation in the cerebrospinal fluid (CSF) of patients with brain tumors were used by researchers.
Both normal and tumor cells regularly release extracellular vesicles, which contain segments of RNA, DNA or proteins and can be found in blood, CSF and other body fluids. A 2008 study from the MGH team was able to identify a relatively large tumor-associated mutation in extracellular vesicles from the blood of brain tumor patients, but most current diagnostic technologies that analyze CSF do not capture molecular or genetic information from central nervous system tumors.
In addition, explains Leonora Balaj, PhD, of MGH Neurology, co-lead author of the current report, "Tumor-specific EVs make up only a small percentage of the total number of EVs found in either blood or cerebrospinal fluid, so finding rare, single-nucleotide mutations in a sample of blood or CSF is very challenging. These digital PCR techniques allow the amplification of such hard-to-find molecules, dramatically improving the ability to identify tumor-specific changes without the need for biopsy."
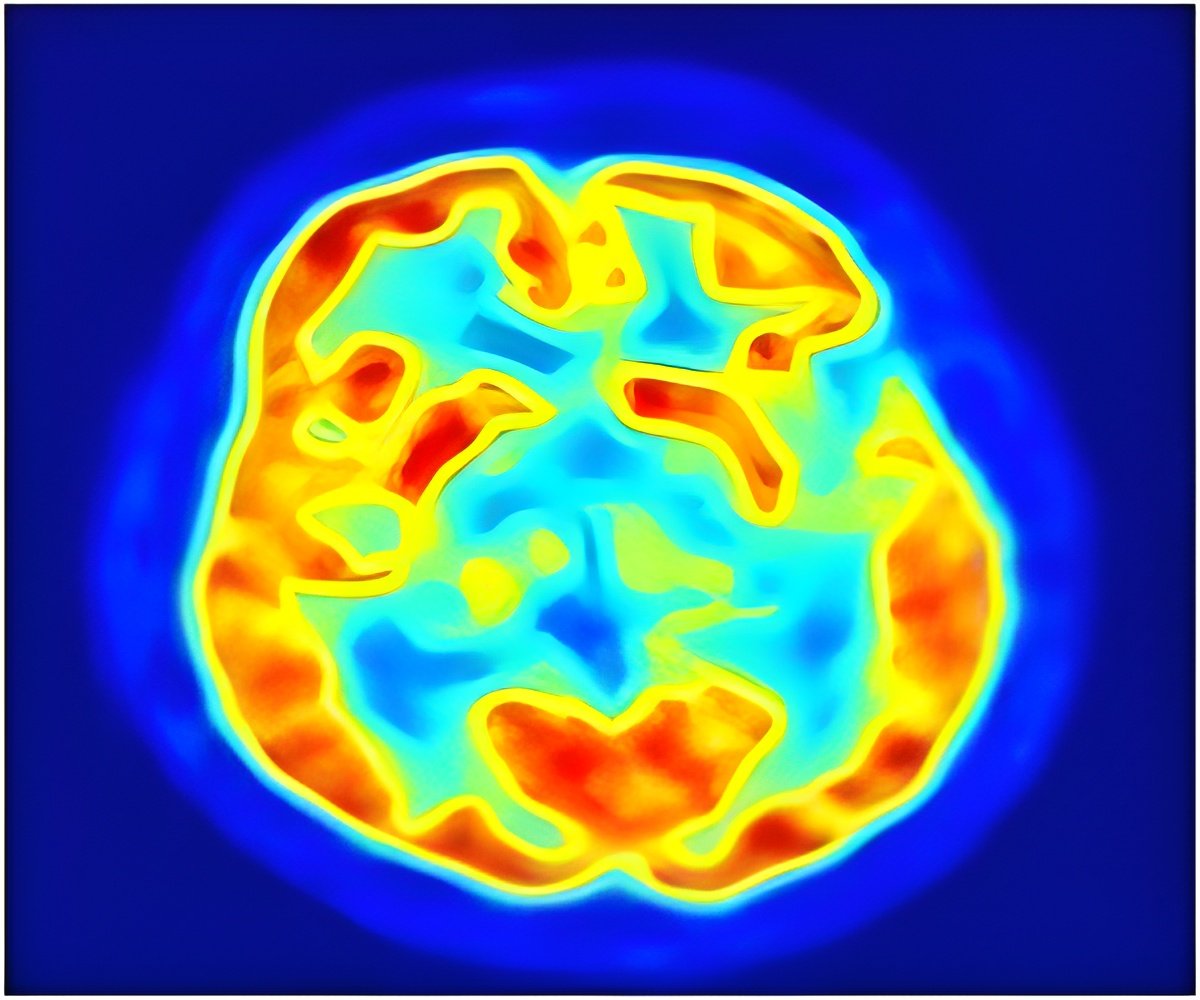
The current study used two forms of digital PCR – BEAMing and Droplet Digital PCR – to analyze extracellular vesicles in the blood and CSF of brain tumor patients and healthy controls for the presence of a single-nucleotide IDH1 mutation known to be associated with several types of cancer. Both forms of PCR were able to detect both the presence and abundance of mutant IDH1 in the CSF of 5 of the 8 patients known to have IDH1-mutant tumors. Two of the three mutation-positive tumors that had false negative results were low grade and the third was quite small, suggesting a need for future studies of more samples to determine how the grade and size of the tumors affect the ability to detect mutations. The failure to detect tumor-associated mutations in blood samples with this technology may indicate that CSF is a better source for extracellular vesicles from brain tumors.
The ability to noninvasively determine the genetic makeup of brain tumors could have a significant effect on patient care, explains study co-author Fred Hochberg, MD, MGH Neurology. "The current approach for patients who may have a brain tumor is first to have a brain scan and then a biopsy to determine whether a growth is malignant. Patients may have a second operation to remove the tumor prior to beginning radiation therapy and chemotherapy, but none of these treatments are targeted to the specific molecular nature of the tumor."
Advertisement
Breakefield is a professor of Neurology at Harvard Medical School, where Hochberg is an associate professor and Balaj a research fellow, also in Neurology. Walter Chen, MGH Neurology, is also co-lead author of the Molecular Therapy – Nucleic Acid paper. Additional co-authors are Casey Maguire, Li Dan Zhu, and Sarada Sivaraman, MGH Neurology; Linda Liau, Horacio Soto, and Matthew Garrett, University of California, Los Angeles; Michael Samuels and Steven Kotsopoulos, RainDance Technologies; Lori LoGuidice and Johan Skog, Exosome Diagnostics; Clark Chen and Eric Wong, Beth Israel Deaconess Medical Center; and Bob Carter, University of California, San Diego.
Advertisement
Source-Eurekalert














