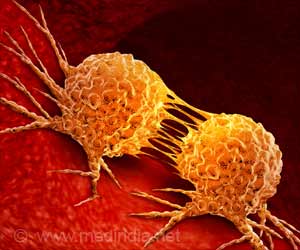
Development of therapies that lead to disruption of protein production or translation, vital for the survival and growth of cancer cells, can dramatically slow down tumor growth.
"In a perverted twist of fate, cancer cells take advantage of this incredibly ancient survival strategy-the heat shock response-to help them survive despite the best efforts of our own natural defenses, and sophisticated therapeutics, to kill them," says Whitehead Member Susan Lindquist. "And trumping all that, we find it not only helps them survive, it helps them thrive!"
Across tumor and cancer types, cancer cells rely on the heat shock response and HSF1 to support the production of vast quantities of proteins and the high-energy demands needed to propel malignancy. Accordingly, researchers have envisioned HSF1 as a potential therapeutic target, but such transcriptional regulators have been notoriously difficult to target. However, by determining that protein translation is intimately connected to HSF1 activity, Whitehead scientists may have identified an approach to controlling cancer cells' overactive heat shock response. Their work is described in this week's issue of the journal Science.
"The genetic screens that we conducted in collaboration with the Broad Institute and the drug screens that were conducted by Sandro Santagata (Lindquist lab postdoctoral researcher) all pointed to this connection-that the process of protein production signals to HSF1," says Marc Mendillo, a postdoctoral researcher in Lindquist's lab and a coauthor of the Science paper with Santagata. "And this link may explain the HSF1 activation we have observed across an extraordinarily broad range of human cancers."
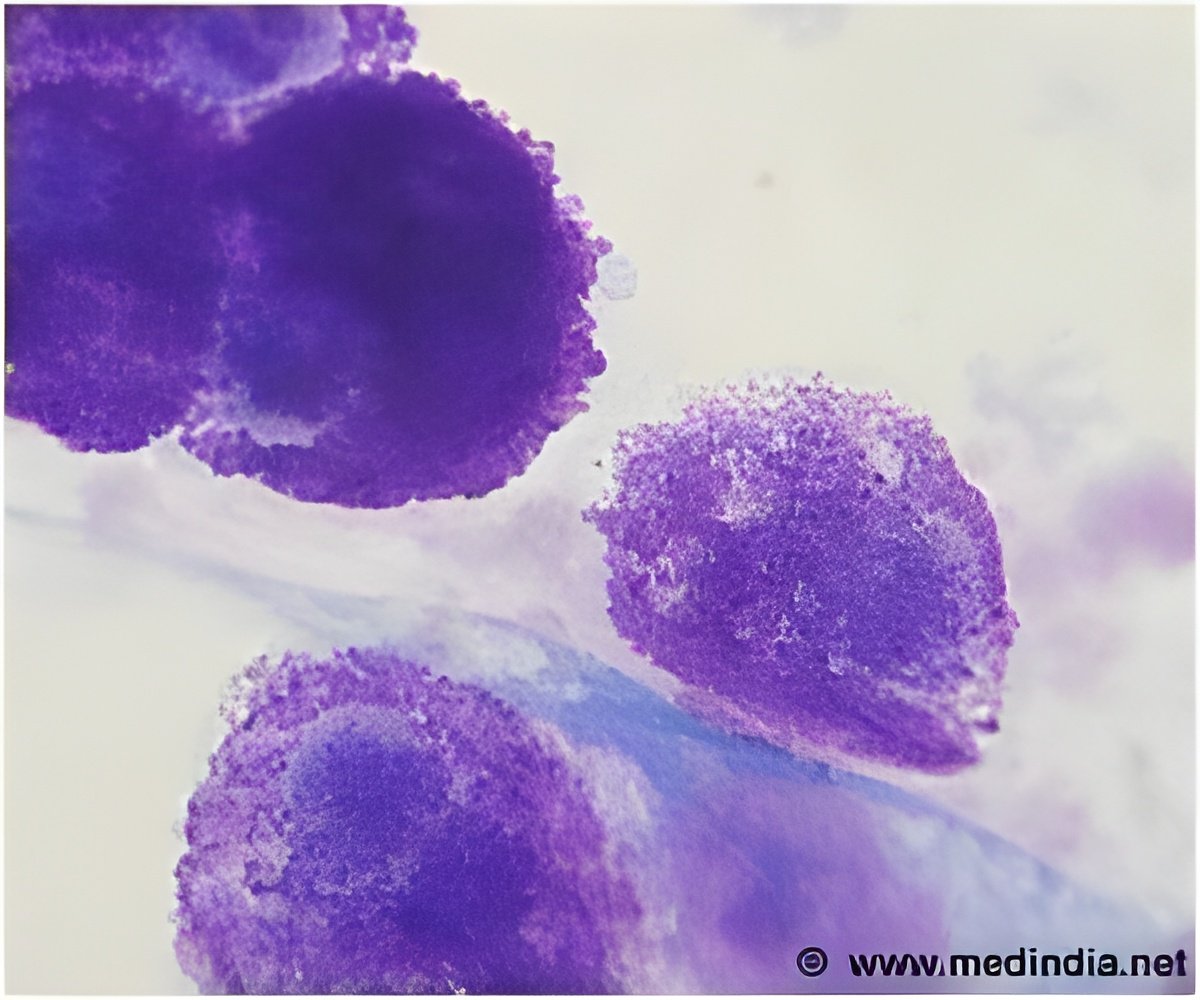
Santagata's screens identified one compound that was particularly effective at disrupting translation and HSF1 activity. Collaborators at Boston University synthesized an analog of this compound, called Rohinitib (RHT), that is even more efficacious. Normal cells are relatively resistant to RHT and seem to be little affected by it. However, cells from a wide spectrum of cancers are sensitive to it-RHT added to cancer cells in vitro normalizes their metabolism, including the increased glucose uptake characteristic of such cells, and even kills them. Blood cancer lines are highly sensitive to RHT and show the most dramatic effects. In mice implanted with human myeloid leukemia tumors, RHT greatly inhibited the tumors' growth and suppressed glucose uptake, similar to the effects seen in vitro.
"I think we've found a very simple but elegant biological principle here, which makes sense," says Santagata. "Systems in the cell that need to work together-such as protein translation and the heat shock response-actually are linked together. We found that link using small molecules, which means that we now have the tools in hand to suppress what cancer has coopted. We can use those chemicals to thwart the cancer cells' ability to harness the properties of HSF1."
Advertisement
"You probably want to have these kinds of effects in the context of other therapeutic interventions," says Luke Whitesell, an oncologist and senior research scientist in the Lindquist lab. "If you were to compromise the altered physiology of tumors with something like RHT, the cancer cells are going to be less able to tolerate other therapeutic insults, and that probably would give you more effective therapies. But we don't know what the best combinations are going to be yet."
Advertisement
Written by Nicole Giese Rura
Susan Lindquist's primary affiliation is with Whitehead Institute for Biomedical Research, where her laboratory is located and all her research is conducted. She is also a Howard Hughes Medical Institute investigator and a professor of biology at Massachusetts Institute of Technology.
Full Citation:
"Tight Coordination of Protein Translation and HSF1 Activation Supports the Anabolic Malignant State"
Science, July 18, 2013
Sandro Santagata (1,2,3,*), Marc L. Mendillo (3,4,*), Yun-chi Tang (4,5, ), Aravind Subramanian (6), Casey C. Perley (3,4), Stéphane P. Roche (7), Bang Wong (6), Rajiv Narayan (6), Hyoungtae Kwon (3,4), Martina Koeva (3,4), Angelika Amon (4,5), Todd R. Golub (6), John A. Porco Jr. (7), Luke Whitesell (3), and Susan Lindquist (3,4).
1. Department of Pathology, Brigham and Women's Hospital (BWH), and Harvard Medical School, Boston, MA, USA.
2. Dana Farber Cancer Institute, Boston, MA, USA.
3. Whitehead Institute for Biomedical Research (WIBR), Cambridge, MA, USA.
4. Howard Hughes Medical Institute, Department of Biology, Massachusetts Institute of Technology (MIT), Cambridge, MA, USA.
5. David H. Koch Institute for Integrative Cancer Research and Howard Hughes Medical Institute, MIT, Cambridge, MA, USA.
6. Broad Institute of MIT and Harvard, Cambridge, MA, USA.
7. Department of Chemistry, Center for Chemical Methodology and Library Development (CMLD-BU), Boston University, Boston, MA, USA.
*These authors contributed equally to this work.
Present address: Institute of Health Sciences, Shanghai Institutes for Biological Sciences, Chinese Academy of Sciences & Shanghai Jiao Tong University School of Medicine, Shanghai, China.
Source-Newswise