The exact process of chronic lymphocytic leukemia patients developing resistance to ibrutinib, a highly effective, precisely targeted anti-cancer drug, has been understood.
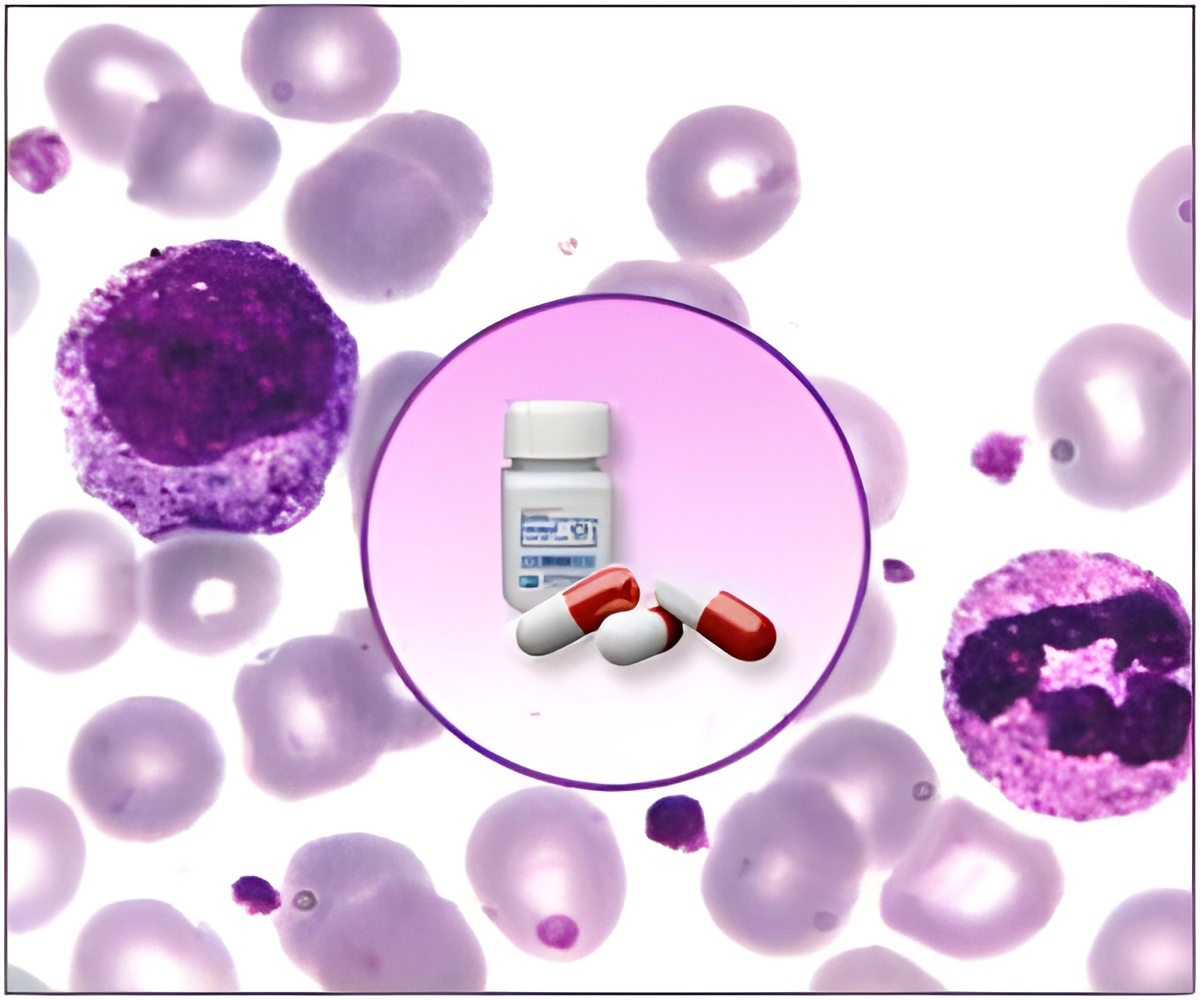
In this study, the researchers describe a point mutation in one participant enrolled in a multi-center clinical trial. This patient stopped responding to treatment after almost 20 successful months. The mutation destabilized the binding of ibrutinib to its target, a protein that regulates cell replication, allowing leukemic cells to multiply freely.
"In a way, we are repeating, at a faster pace, the story of Gleevec (imatinib), a landmark drug that transformed care for a different type of leukemia," said study senior author Y. Lynn Wang, MD, PhD, professor of pathology at the University of Chicago. "That story began with development of an effective drug with few side effects, but in many patients the leukemia eventually found a way around it after long-term use. So researchers developed second-line drugs to overcome resistance."
The ibrutinib study began in 2010 at Weill Cornell Medical College in New York City, one of several sites for a phase 1 clinical trial of ibrutinib. The researchers recruited 16 patients with CLL whose disease had progressed or relapsed despite multiple treatments.
Wang, who recently moved from Cornell to the University of Chicago, arranged to track the progress of each patient's leukemic cells before and during treatment and to correlate any cellular or molecular changes with each patient's disease activity.
One of the 16 patients in the trial seemed to be unusual. This 61-year-old woman was diagnosed in 2000 at age 49. She had unsuccessfully received several different treatments before entering the study. Within 18 months after starting ibrutinib, she showed significant improvement. At about 20 months, however, she started to decline, developing a respiratory infection that did not improve with treatment. By 21 months it was clear she was having a relapse. The clinical team increased her dose, with no discernable effect.
Advertisement
Complete gene sequencing and analysis can take a long time so Wang asked a graduate student working on the project, Menu Setty from Christina Leslie's Laboratory at Memorial Sloan Kettering, to focus at first on three proteins, all likely candidates. She gave him the assignment over the July 4, 2012, holiday. On July 5 he had the answer.
Advertisement
BTK made perfect sense as the cause for drug resistance. It is the primary target of ibrutinib binding and it plays a central role in rapid cell proliferation, as demonstrated in a previous publication by Wang's group and others.
Her team used structural and biochemical measures to confirm that it was this small change in the DNA that made CLL cells resistant to the drug. Biochemical studies indicate that ibrutinib was 500 times less likely to bind to mutant BTK.
In an attempt to save the patient, the team also tested alternative kinase inhibitors against the patient's leukemic cells in the laboratory. They found some kinase inhibitors remained effective against ibrutinib-resistant cells. (These studies are described in a separate manuscript that has been submitted for publication.) Despite the effort, the patient passed away a few weeks later from sepsis.
Although the BTK mutation is one of several mechanisms that underlie resistance to ibrutinib, this study highlights its role in disease development and drug resistance, the authors note. Understanding the molecular and cellular mechanisms of resistance is the first step toward monitoring, early detection and development of novel strategies to overcome drug resistance.
The Leukemia and Lymphoma Society and the Prince Family Foundation funded this research. Additional contributors include Pin Lu and Ailin Guo from the University of Chicago; Richard Furman, Shuhua Cheng, Joelle Racchumi, Jia Ma and Morton Coleman from Weill Cornell Medical College; Alijandro Perez and Christina Leslie from Memorial Sloan Kettering Cancer Center; Guozhou Xu and Hao Wu from Boston Children's Hospital; and Susanne Steggerda from Pharmacyclics Inc., the makers of ibrutinib (marketed as Imbruvica).
Source-Newswise