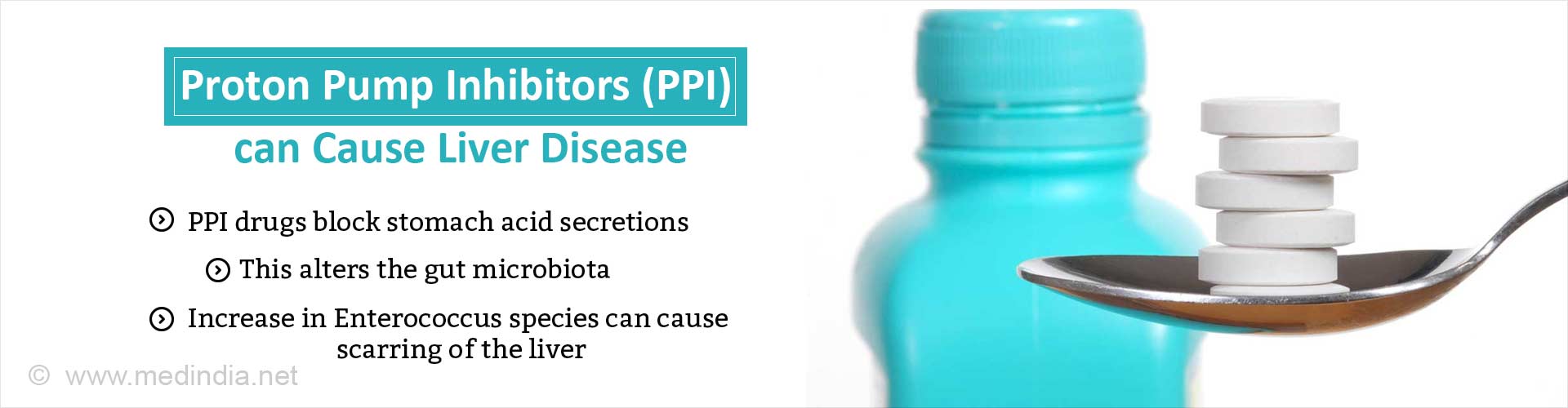
Proton pump inhibitors prescribed for heartburn, acid reflux can alter the gut microbiota and increase the risk of chronic liver injury.
Highlights
- Drugs that block the secretion of gastric acids can increase risk of chronic liver disease.
- Proton pump inhibitor (PPI) drugs block stomach acid secretions and relieve symptoms of frequent heartburn, acid reflux.
- Gastric acid suppression alters specific gut bacteria in a way that promotes liver injury and progression of three types of chronic liver disease.
The absence of gastric acid promotes growth of Enterococcus bacteria in the intestines and translocation to the liver, where they exacerbate inflammation and worsen chronic liver disease.
Proton Pump Inhibitors May Trigger Liver Disease
Schnabl’s team looked at mouse models that mimic alcoholic liver disease, non-alcoholic fatty liver disease (NAFLD) and steatohepatitis (NASH) in humans to determine the effect of gastric acid suppression on the progression of chronic liver disease.
The gastric acid production was blocked either by genetic engineering or with a PPI (omeprazole/Prilosec). Microbe-specific genes collected from the animals’ stool was sequenced to determine the gut microbiome makeup of each mouse type, with or without blocked gastric acid production.
Mice with gastric acid suppression developed alterations in their gut microbiomes. Specifically, they had more Enterococcus species of bacteria. These changes promoted liver inflammation and liver injury, increasing the progression of all three types of liver disease in the mice: alcohol-induced liver disease, NAFLD and NASH.
Increased Enterococcus alone was sufficient to induce mild steatosis and increase alcohol-induced liver disease in mice.
From a cohort of 4,830 patients with a diagnosis of chronic alcohol abuse -- 1,024 (21 percent) were active PPI users, 745 (15 percent) were previous users and 3061 (63 percent) had never used PPIs.
PPI intake among these patients increased stool concentrations of Enterococcus. The 10-year risk of a diagnosis of alcoholic liver disease was 20.7 percent for active users of PPIs, 16.1 percent for previous users and 12.4 percent for never users.
In other words, the rate of liver disease in people who chronically abuse alcohol was 8.3 percent higher for those who actively use PPIs compared to those who never used the acid-blocking medications.
Though there could be other unidentified factors that differ between patients that do and do not take PPIs, there is an association between PPI use among people who abuse alcohol and risk of liver disease.
Bottom line
The initial data should at least get people thinking about reducing their use of PPIs in cases where they aren’t a necessity and can use non-PPI-based antacids (e.g., Pepto-Bismol, Tums, or H2 blockers such as Tagamet and Zantac).
Alternatively, non-pharmacological methods for managing heartburn are an option for some patients, including losing weight and reducing intake of alcohol, caffeine, and fatty and spicy foods.
"Although obesity and alcohol use predispose a person to acid reflux requiring antacid medication, many patients with chronic liver disease take gastric acid suppressive medications without appropriate indication. We believe clinicians should consider withholding medications that suppress gastric acid unless there is a strong medical indication."
As the study was done on mouse models and using a large database, clinical trials are necessary to confirm the findings.
"We might someday be able to manipulate the gut microbiome, and in particular Enterococcus fecalis, to attenuate alcohol-related liver disease associated with gastric acid suppression," Schnabl said.
Reference
- Bernd Schnablet al.Gastric acid suppression promotes alcoholic liver disease by inducing overgrowth of intestinal Enterococcus, Nature Communications http://dx.doi.org/10.1038/s41467-017-00796-x.
Source-Medindia