A new study has found that early stem cell transplants may not improve survival in high-risk patients with aggressive non-Hodgkin's lymphoma.
Lead author is Patrick Stiff, MD, director of Loyola University Medical Center's Cardinal Bernardin Cancer Center. The study was developed by the SWOG cancer research cooperative group and funded by the National Cancer Institute. Stiff is chair of the SWOG Bone Marrow and Stem Cell Transplantation Committee.
The traditional first-line therapy for aggressive non-Hodgkin's lymphoma is a combination of four chemotherapy drugs. In recent years, physicians have added a fifth drug, the monoclonal antibody rituximab. This five-drug regimen is known as R-CHOP. The treatment typically puts patients into remission. But many patients relapse and go on to get an autologous stem cell transplant after second-line chemotherapy.
The study was designed to determine whether doing an early stem cell transplant – without first waiting to see whether a patient relapses -- would increase survival.The clinical trial included 40 sites in the United States and Canada. In addition to SWOG, the study included the Eastern Cooperative Oncology Group, Cancer and Leukemia Group B and Canadian NCIC Clinical Trials Group.
The study included 397 patients who were in defined groups of high risk or intermediate-high risk of relapsing. After initial chemotherapy, those who responded were randomly assigned to receive an autologous stem cell transplant (125 patients) or to a control group of 128 patients who received three additional cycles of the R-CHOP regimen. Enrollment began in 1999 and ended in 2007. (Some of the patients in the beginning of the study did not receive rituximab.)
After two years, 69 percent of the transplantation patients had no disease progression, compared with 55 percent of the control group -- a statistically significant difference. However, the difference in two-year survival rates (74 percent in the transplantation group and 71 percent in the control group) was not statistically significant. This is probably because patients in the control group who relapsed were later offered stem cell transplants, Stiff and colleagues wrote.
Advertisement
"Early transplantation and late transplantation achieve roughly equivalent overall survival in the combined risk groups," researchers concluded, yet "early transplantation appears to be beneficial for the small group of patients presenting with high-risk disease."
Advertisement
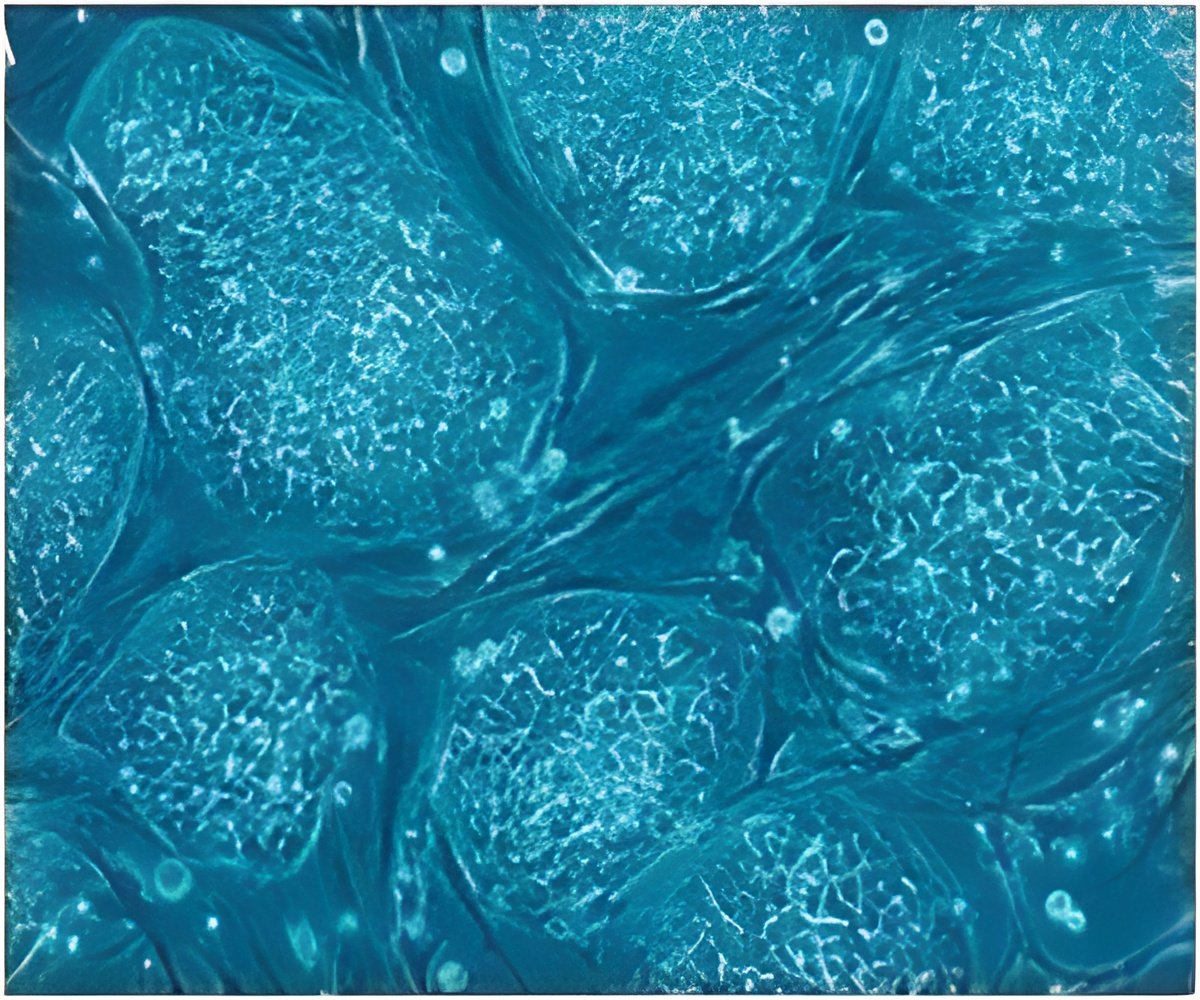
An autologous stem cell transplant enables a patient to tolerate very high doses of chemotherapy and/or radiation. In addition to killing cancer cells, this high-dose treatment also destroys the patient's immune system cells. So prior to treatment, stem cells are removed from the patient's blood or bone marrow. After the chemotherapy and/or radiation, these stem cells are infused back into the patient. The stem cells develop into new immune cells, replacing the immune cells destroyed by the treatment.
Previous studies have found that patients who undergo stem cell transplants have a slightly higher risk of developing secondary cancers caused by the chemotherapy and/or radiation. However, the new study did not find a statistically significant difference – 11 patients in the control group developed secondary cancer, compared with 12 patients in the transplantation group.
Researchers are continuing to analyze the data. "As years go by, there may be additional analysis that may help fine-tune the results so that we will be able to more carefully and concisely define any potential benefit of transplant," Stiff said.
Source-Eurekalert