The ultimate aim is to provide more accurate diagnoses for all patients, thus directing appropriate rehabilitation an therapy to those most likely to benefit.
‘EEG assessment may be capable of diagnosing a patient's level of awareness without the need for expensive and challenging fMRI scans, thereby increasing the number of patients who may benefit from a more accurate diagnosis.’





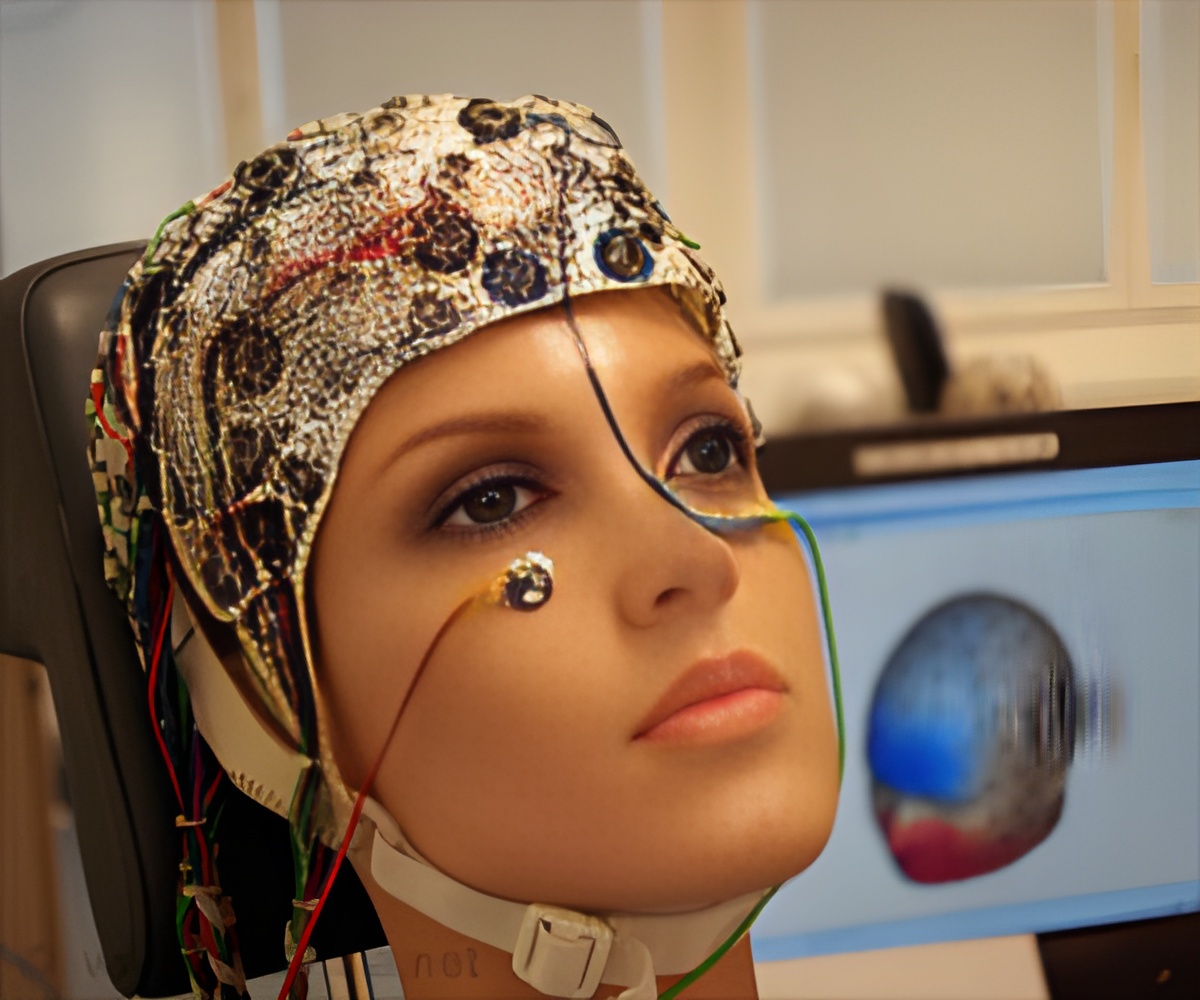
The new research findings, published in Annals of Neurology, suggest a correspondence between a patient's ability to generate an EEG marker of attention to tactile stimulation, and their ability to produce the critical clinical marker of awareness by following verbal commands. Crucially, this relationship existed for patients who could only follow commands with the more expensive methods of fMRI. The mental demands of the EEG task are lower than the demands of the fMRI tasks. Furthermore, EEG is entirely portable, inexpensive, and available in the majority of hospitals.
The researchers state that this more simple EEG assessment may be capable of diagnosing a patient's level of awareness without the need for expensive and challenging fMRI scans, thereby increasing the number of patients who may benefit from a more accurate diagnosis.
14 patients were selected for the study, across levels of awareness and behavioural ability; seven in a vegetative state, four in a minimally conscious state, two emerging from a minimally conscious state, and one with locked in syndrome.
Each patient's surrogate decision maker provided informed, written consent for the patient's participation in the study. As a scientific control, a sample of fifteen healthy volunteers also participated in the tasks.
Advertisement
Vibrating stimulators affixed to each wrist and the upper back administered non-painful pulses five times per second while the patients' EEGs were recorded. 80% of these vibrations occurred on the upper back. The relatively more infrequent vibrations on the wrists (20% of the time) produce changes in a healthy individual's EEG that reflect attention being drawn toward the new location of stimulation.
Advertisement
All patients whose EEGs showed evidence of attention being directed toward the infrequent tactile stimuli were also able to display evidence of following commands in the fMRI tasks. Similarly, most patients (five of six) who did not generate a response to the EEG task did not generate evidence of command following.
Dr Damian Cruse, from the University of Birmingham, explained, "A bedside EEG may work as a cost-efficient and portable way of improving the accuracy of diagnosis in disorders of consciousness. While current clinical diagnoses are accurate for many patients, recent reports estimate that as many as 15% of patients considered to be in a vegetative state could retain awareness that cannot be detected reliably from their behaviour alone." The ultimate aim is to provide more accurate diagnoses for all patients, thus directing appropriate rehabilitation and therapy to those most likely to benefit.
Source-Eurekalert