A three drug model of therapy designed by researchers from The University of Warwick will aid in rapid treatment of elephantiasis, eliminating the disease by 2020.
Highlights
- New model of therapy for elephantiasis using three drugs developed.
- A combination of the three drug therapy treats the disease rapidly and WHO hopes to eliminate lymphatic elephantiasis by 2020.
- The three drugs are ivermectin, diethylcarbamazine and albendazole and drug companies Merck, GlaxoSmithKline and Eisai have pledged to provide free drugs.
Elephantiasis
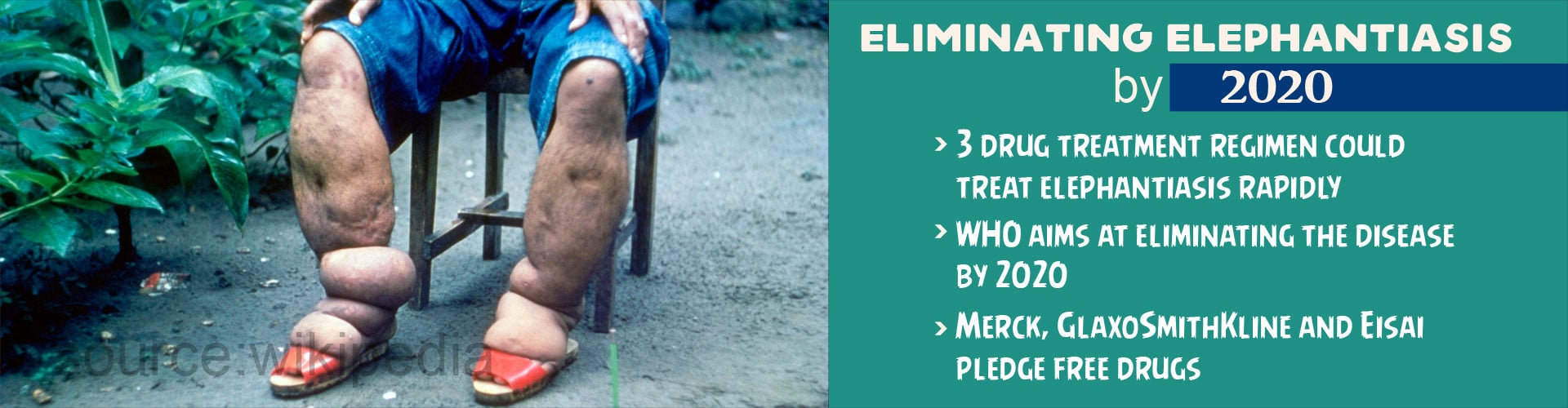
Elephantiasis is also called lymphatic filariasis, and is caused by parasitic worms. Mosquitoes are vectors for the disease. This disease condition is characterized by gross enlargement of a part of the body, especially the limbs. The external genitals are other areas that are commonly affected.The lymphatic system includes a network of tubular channels that are called the lymph vessels. These vessels drain a thin watery fluid called the lymph from various parts of the body and when such a lymph node is blocked, the lymph begins to accumulate, resulting in the characteristic symptom of the disease.
The enlargement of the body part that occurs can be painful and can be disfiguring, sometimes even leading to permanent damage. This could result in the individual feeling socially stigmatized apart from the monetary and physical strain on the individual.
Countries at High Risk
80% of the disease is found in countries like India, Indonesia and Myanmar, Angola, Democratic Republic of Congo, Nigeria, Mozambique, Cameroon, Cote D’Ivoire and The United Republic of Tanzania.- 1 billion people are at high risk
- People in over 54 countries are at some risk of being infected
- In the year 2000, 120 million were infected and 40 million disfigured
The current treatment methodology for lymphatic filariasis involves many rounds of drugs. However, the current study includes a combination of three drugs, ivermectin, diethylcarbamazine and albendazole that are found to be more effective and treat the disease rapidly. These require only two to three rounds of administration as against the previous drug regimen that was administered for multiple rounds.
Pledge to Eradicate Lymphatic Filariasis
The World Health Organization (WHO) is working towards eliminating the disease by year 2020. Three drug companies have pledged their support and offered to provide free drugs to eliminate the disease - Merck, GlaxoSmithKline and Eisai.The use of triple drugs in treating the disease is far more effective and rapid when compared with a single drug approach. However, the researchers are a little apprehensive about how effective the distribution and the use of the drug would be. People seldom stick to drug regimens when the disease is rare.
Dr. Hollingsworth who is based in The University of Warwick’s Mathematic Institute and School of Life Sciences stated that the effectiveness of the treatment was dependent on being able to reach the most inaccessible people. This will truly aid in lowering incidence of the disease.
The first author of the study, Dr. Mike Irvine from the University of British Columbia says that the important aspect of elimination campaigns is to find an effective treatment method that will lower the risk of the disease within a few years, long drawn treatment modules will not be effective.
“The multi-modelling study could aid the Indian policy makers to decide on the need for introducing the triple drug regimen in the ‘hard-core’ districts to accelerate lymphatic filariasis elimination in India“ said Dr. Swaminathan Subramanian, from the Vector Control Research Centre (ICMR).
Elephantiasis due to lymphatic filariasis is a debilitating disease with a strong social stigma attached to it. The efforts taken by the medical fraternity in eliminating this disease condition will aid in removing a dreaded condition that has physically deformed millions till date.
References:
- Lymphatic filariasis - (http://www.who.int/mediacentre/factsheets/fs102/en/)
- Elephantiasis - (https://rarediseases.org/rare-diseases/elephantiasis/)
- Michael A Irvine, Wilma A Stolk, Morgan E Smith, Swaminathan Subramanian, Brajendra K Singh, Gary J Weil, Edwin Michael, T Deirdre Hollingsworth. Effectiveness of a triple-drug regimen for global elimination of lymphatic filariasis: a modelling study. The Lancet Infectious Diseases, 2016; DOI: 10.1016/S1473-3099(16)30467-4