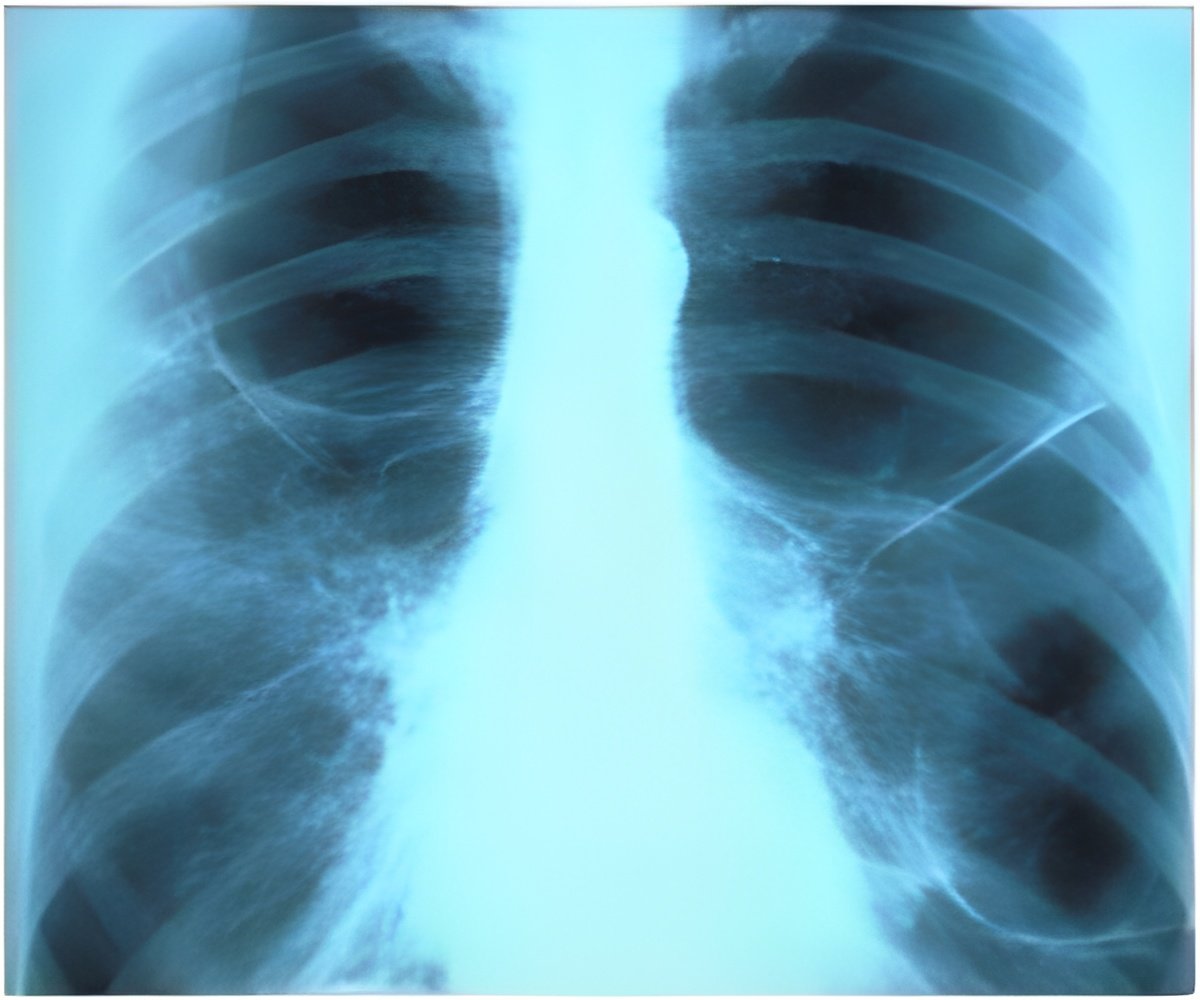
A major cause of pulmonary fibrosis has been pinpointed by Cedars-Sinai investigators.
‘Pulmonary fibrosis results from the failure of special lung stem cells, known as AEC2s, that help airways recover from injury.’





Cedars-Sinai investigators have pinpointed a major cause of pulmonary
fibrosis. The disease, which has no known cure, appears to
result from the failure of special lung stem cells that help airways
recover from injury, the investigators reported in the journal Nature Medicine.
The study is a major step toward understanding and one day treating
pulmonary fibrosis. "Pulmonary fibrosis slowly robs patients of breath and finally life," said Paul W. Noble, professor and chair of the Department of Medicine and director of the Women's Guild Lung Institute at Cedars-Sinai. "In our study, we identified novel potential pathways to finding treatments for this relentless disease." Noble was the study's principal investigator.
The investigators focused on alveoli, the small air sacs at the ends of lung airways. In the alveoli, oxygen and carbon dioxide are exchanged with blood during respiration. Epithelial cells that line the alveoli also make a substance that helps keep the airspaces open. In pulmonary fibrosis, these epithelial cells become abnormal, and fibrous tissue builds up in the lungs, causing severe scarring. Researchers don't know why this scarring process happens.
The Cedars-Sinai research team found an answer in special stem cells known as AEC2s that are found in adult lungs and are critical to repairing and regenerating epithelial cells. When viral infections, pollution or other injuries damage lung tissue, AEC2 cells come to the rescue.
In people with pulmonary fibrosis, something goes wrong with AEC2 cells, the study found. Compared with lung tissue of disease-free individuals, lung tissue from patients with pulmonary fibrosis had far fewer AEC2 cells, and those that remained were less able to renew themselves. Surfaces of these cells had lower concentrations of hyaluronan, a chemical substance that promotes tissue repair and renewal. Further, in laboratory mice, the team found that by deleting this substance, they could produce the type of scarring found in pulmonary fibrosis after lung injury.
Advertisement
One promising approach may be to develop drugs that stimulate the reproduction of AEC2 cells in the lungs of patients who lack enough of these cells, Noble said. "The exciting aspect is that we have learned how to isolate these stem cells from diseased lungs. We can use these cells to create tiny 'lungs in a dish' as tools for drug development," he explained.
Advertisement
Source-Eurekalert