The family trees of cancer cells in acute myeloid leukaemia (AML) have been mapped by researchers.
‘Understanding how clones relate to each other is important as they provide information as to how acute myeloid leukemia started in the first place.’





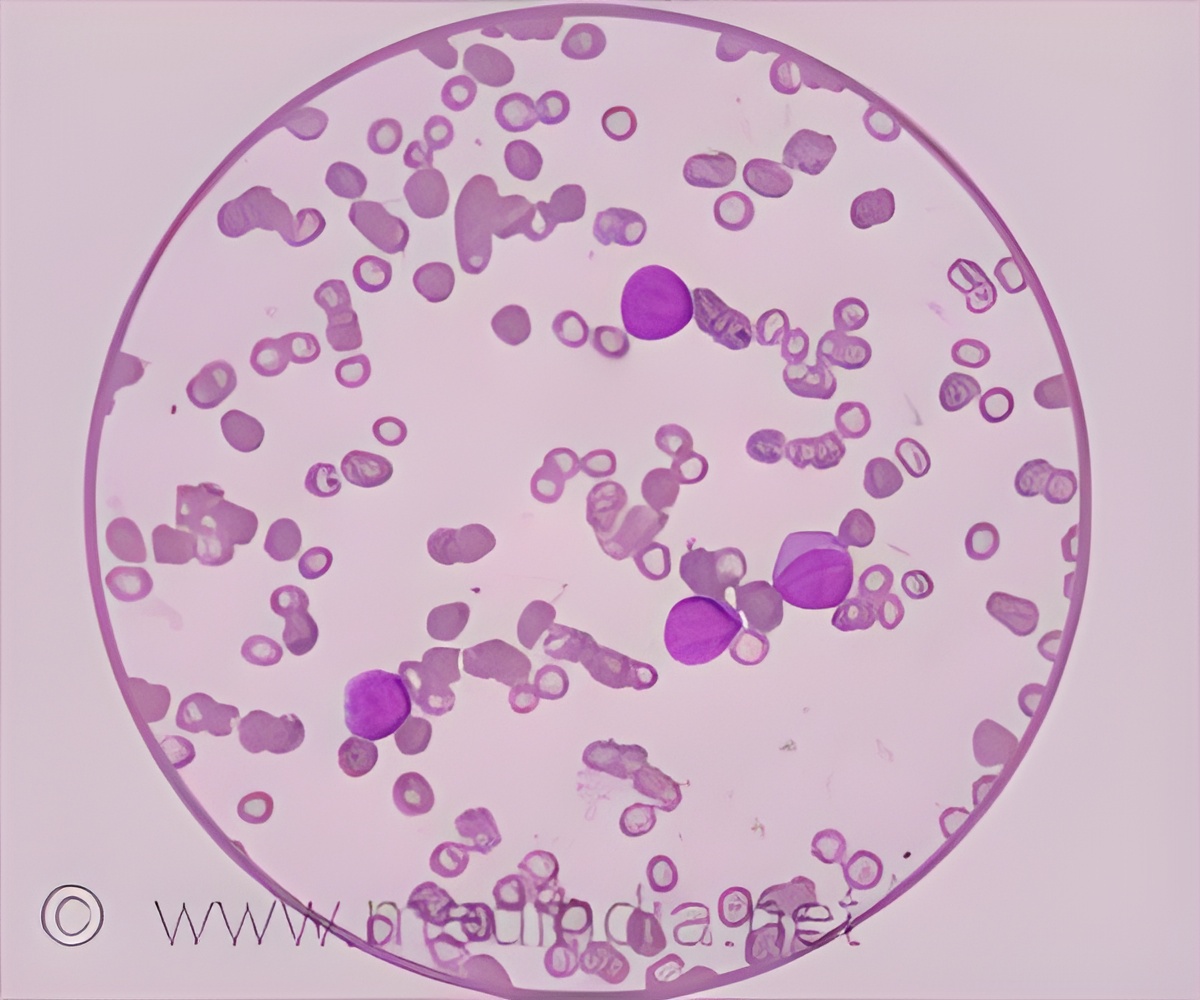
The study published in Nature Medicine is an international collaboration between researchers from the Gustave Roussy Cancer Campus and Inserm in Paris (France), the MRC Molecular Haematology Unit and the MRC Weatherall Institute of Molecular Medicine at the University of Oxford (UK), Memorial Sloan Kettering Cancer Center (USA) and Celgene (USA). AML is the most common and aggressive blood cancer in adults and is incurable in most patients. About 12-15% of AML patients have a mutation in the IDH2 gene that stops bone marrow cells from differentiating, or maturing, into blood cells that are required for life. Instead these immature cells accumulate in the bone marrow and blood, which is a hallmark of AML. Previous research from the same team [2] showed that enasidenib prompts blood cell differentiation and restores normal blood cell production.
A phase I/II clinical trial showed that the drug was effective in 40% of AML patients with an IDH2 mutation who had failed previous treatments. and this led to the US Food and Drug Administration (FDA) giving approval for enasidenib in 2017. However, after an average of nearly nine months, the cancer returned in these patients.
"Enasidenib is an important new treatment. However, the initial studies did not show which AML cells responded to enasidenib and started to differentiate again. It was also unclear how the cells become resistant to therapy," said Dr Stéphane de Botton, physician in the haematology department at Gustave Roussy. "We wanted to answer these questions."
Using samples from 37 patients in the trial who had responded to enasidenib, the team looked at markers on the surface of the bone marrow cells to identify the different populations of bone marrow cells, from the immature, undifferentiated cells, called progenitor cells, through to mature, differentiated cells.
Advertisement
As AML is caused by errors in DNA sequence, or mutations, in blood cells, the team studied the genetic make-up of AML cells. They found that AML cells from the same patient can be grouped into families which share genetic mutations, called clones. Cells belonging to the same clone or family, come from the same ancestor cell.
Advertisement
Co-author, Dr Virginie Penard-Lacronique, research director and team leader at the Inserm unit at Gustave Roussy, said: "We have provided genetic proof that enasidenib was able to differentiate cancer cells so that some of their normal functions were restored, even though they still contained the IDH2 mutation. This is important because unless we can track these clones, we don't know whether the mature cells in a patient are coming from normal cells after all the cancer cells have been killed or from leukaemic cells that are now able to mature. In this paper we show that in four out of five cases, the mature cells are coming from leukaemic bone marrow cells that can be induced to differentiate by this new drug."
The cancer returned in almost all the patients in the clinical trial, and the team was able to show for the first time that the leukaemic cells stop responding to enasidenib when some of the clones develop additional mutations. These new sub-clones are resistant to enasidenib, providing clues about the mechanism of drug resistance. This may help in designing future therapy trials to overcome therapy resistance. It may also mean that enasidenib needs to be combined with other anti-cancer drugs to prevent relapse, and clinical trials have already started investigating whether patients respond to these combinations, for how long and whether they are likely to relapse.
Dr de Botton concluded: "Enasidenib a very good example of a modern cancer therapy that specifically targets principally cancer cells, sparing normal cells, and in this regard is very safe and has limited side effects. Now that we have shown that it needs to be combined with other drugs to stop the cancer returning, we think that it's important that the combination therapy should be given to AML patients early on in their disease. International trials are now taking place comparing combinations of enasidenib and other drugs with the normal standard of care."
Professor Paresh Vyas, professor of haematology and lead of the Oxford team, pointed out: "The approach we have implemented can be applied to any cancer and to any therapy to understand how any drug attacks each clone in a cancer and how different clones respond to therapy. This makes it a very powerful approach to improve our understanding of how to achieve better outcomes from cancer therapy."
Source-Eurekalert