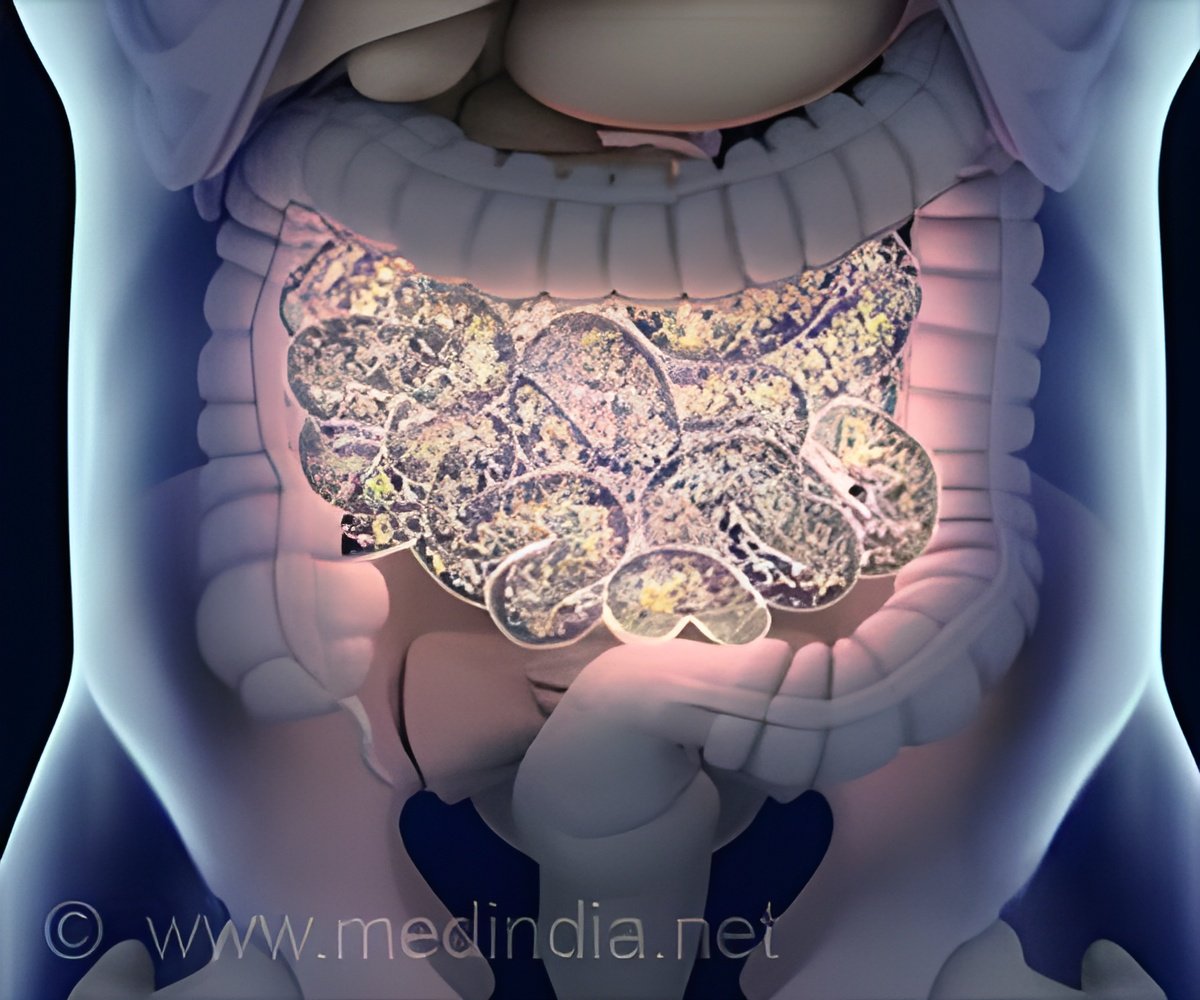
Exploring fecal, blood, and urinary biomarkers to enhance diagnosis and monitoring of inflammatory bowel diseases, offering non-invasive alternatives to traditional methods.
Fecal, Blood, and Urinary Biomarkers in Inflammatory Bowel Diseases
Go to source) These conditions primarily impact older adults and show significant geographic variation, with higher rates in developed countries. While ileo-colonoscopy remains the gold standard for diagnosing and monitoring IBD, its invasive nature and limited availability result in long patient wait times. As a result, there is growing interest in finding non-invasive biomarkers to better assess disease activity.
‘Fecal calprotectin and C-reactive protein are key biomarkers for inflammatory bowel diseases, closely linked to disease activity and treatment response. #IBD #Crohnsdisease’





Biomarkers are measurable compounds or substances that can be quantitatively evaluated in biological samples such as blood, urine, tissue, or feces. Recent research has focused on developing biomarkers that can assess disease activity, predict disease course, and monitor therapeutic response in IBD patients. The most relevant biomarkers studied include fecal calprotectin (FC) and C-reactive protein (CRP). Fecal Calprotectin (FC): A Promising Biomarker for Non-Invasive IBD Monitoring
FC is a cytosolic calcium and zinc-binding protein expressed by neutrophils and other immune cells. It is a stable protein that can persist in feces for up to a week, making it an ideal biomarker for non-invasive monitoring. FC has been extensively studied in IBD and has shown good-to-optimal correlation with endoscopic, histologic, and transmural disease activity. Several studies have reported high sensitivity and specificity of FC in differentiating IBD from healthy controls and functional gastrointestinal disorders. FC has also been shown to accurately predict endoscopic disease activity, reducing the need for colonoscopy in many cases.CRP is an acute-phase reactant protein produced by the liver in response to inflammation. Its levels are often elevated in IBD patients, particularly during active disease phases. CRP has been used as a biomarker to monitor disease activity and predict treatment response. While CRP alone may not be as specific as FC, it can provide valuable information when combined with other biomarkers and clinical indices.
Research has also explored the potential advantages of using multi-target tools that combine serum and fecal biomarkers with clinical activity indexes. These tools aim to enhance diagnostic and monitoring effectiveness by providing a more comprehensive picture of disease status. Fecal lactoferrin, autoantibodies, microRNAs, gene expression, and other serological and fecal markers have shown promising results but require further validation before widespread adoption in clinical practice.
The implementation of the "treat-to-target" strategy in IBD management has heightened the significance of biomarkers. This approach involves meticulously pursuing multiple therapeutic objectives, which relies on periodic monitoring of markers of disease activity. Studies such as the CALM trial have demonstrated that promptly escalating treatment guided by both clinical symptoms and biomarkers yields superior clinical and endoscopic outcomes in IBD patients. The STRIDE-II consensus initiative has also emphasized the importance of clinical response, remission, endoscopic healing, and normalization of CRP/erythrocyte sedimentation rate and FC as primary therapeutic targets.
Advertisement
The incidence and prevalence of IBD continue to rise globally, necessitating the development of non-invasive diagnostic and monitoring tools. Multi-target tools that combine biomarkers with clinical indices have also shown promising results. Further research is needed to validate these biomarkers and incorporate them into routine clinical practice to improve the management of IBD patients.
Advertisement
- Fecal, Blood, and Urinary Biomarkers in Inflammatory Bowel Diseases - (https://www.xiahepublishing.com/2994-8754/JTG-2024-00001)













