For couples with unexplained infertility, sperm diagnostic test may help determine the best infertility treatment for couples having difficulty conceiving.

Published in Science Translational Medicine, "Absence of sperm RNA elements correlates with idiopathic male infertility," by the laboratory of Stephen Krawetz, Ph.D., associate director of the C.S. Mott Center for Human Growth and Development and the Charlotte B. Failing Professor of Fetal Therapy and Diagnosis in the WSU Department of Obstetrics and Gynecology - with Dr. Meritxell Jodar, Edward Sendler, Robert Goodrich, Dr. Clifford Librach, Dr. Sergey Moskovtsev and Sonja Swanson of CreATe Fertility Center, University of Toronto; Dr. Russ Hauser of Harvard University and Dr. Michael Diamond of Georgia Regents University - details how male factors could be the cause of infertility in couples even when tested semen parameters are normal.
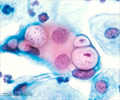
The use of next-generation sequencing of spermatozoal ribonucleic acids, or RNAs, can provide an objective measure of the paternal contribution, and may help guide couples to the most effective method in overcoming infertility.
"Upon validation, this discovery may help to identify those couples who may benefit from assisted reproductive technologies and those couples who may be successful with minimal intervention," said Dr. Krawetz, also a professor of Molecular Medicine and Genetics. "It is our goal to use this technology to reduce both the time to live birth of a healthy child and the cost when couples seek infertility treatment, so as to reduce the stress on the couple. It is our hope that by identifying the extent of the father's contribution, the responsibility for setting the course for the birth of a healthy child can now be more equally shared."
These new findings hold the possibility of dramatic changes in the way infertile couples are treated and assisted in achieving pregnancy. About 13 percent of couples of reproductive age experience fertility problems. While the American Society for Reproductive Medicine estimates that male and female factors contribute about equally to infertility, extensive evaluation of the female partner is traditional before undergoing fertility treatments.
Evaluation of the male partner is not as extensive, and is generally relegated to a review of reproductive history, family history and semen analysis considering parameters that include sperm concentration, motility and morphology. The semen parameters evaluation may be useful in the diagnosis of obvious cases of male infertility, Dr. Krawetz said, but no single parameter or set of parameters serve as highly predictive of male fertility. Results of those tests are limited in helping select the least invasive fertility treatment for couples having difficulty conceiving.
The diagnostic potential of next-generation sequencing of spermatozoal RNA indicates this method is "better suited to the task" of analyzing the male's role in infertility, and is a step toward personalized precision reproductive medicine that may help guide the couple to their successful treatment, Dr. Krawetz said.
Sperm RNA analysis at present is technically challenging, but it is being automated. The technique could become part of a routine examination as "we move toward personalized and precision medicine," Dr. Krawetz said. While the test is experimental, it has the potential for cost savings for both the patients and the health care system.
The next step is to expand to a prospective blinded study and to begin to define a set of markers that may be predictive of assisted reproduction outcomes.
Source-Medindia