The overall five-year relative rate of survival for pancreatic cancer is around 6 percent, according to the National Cancer Institute
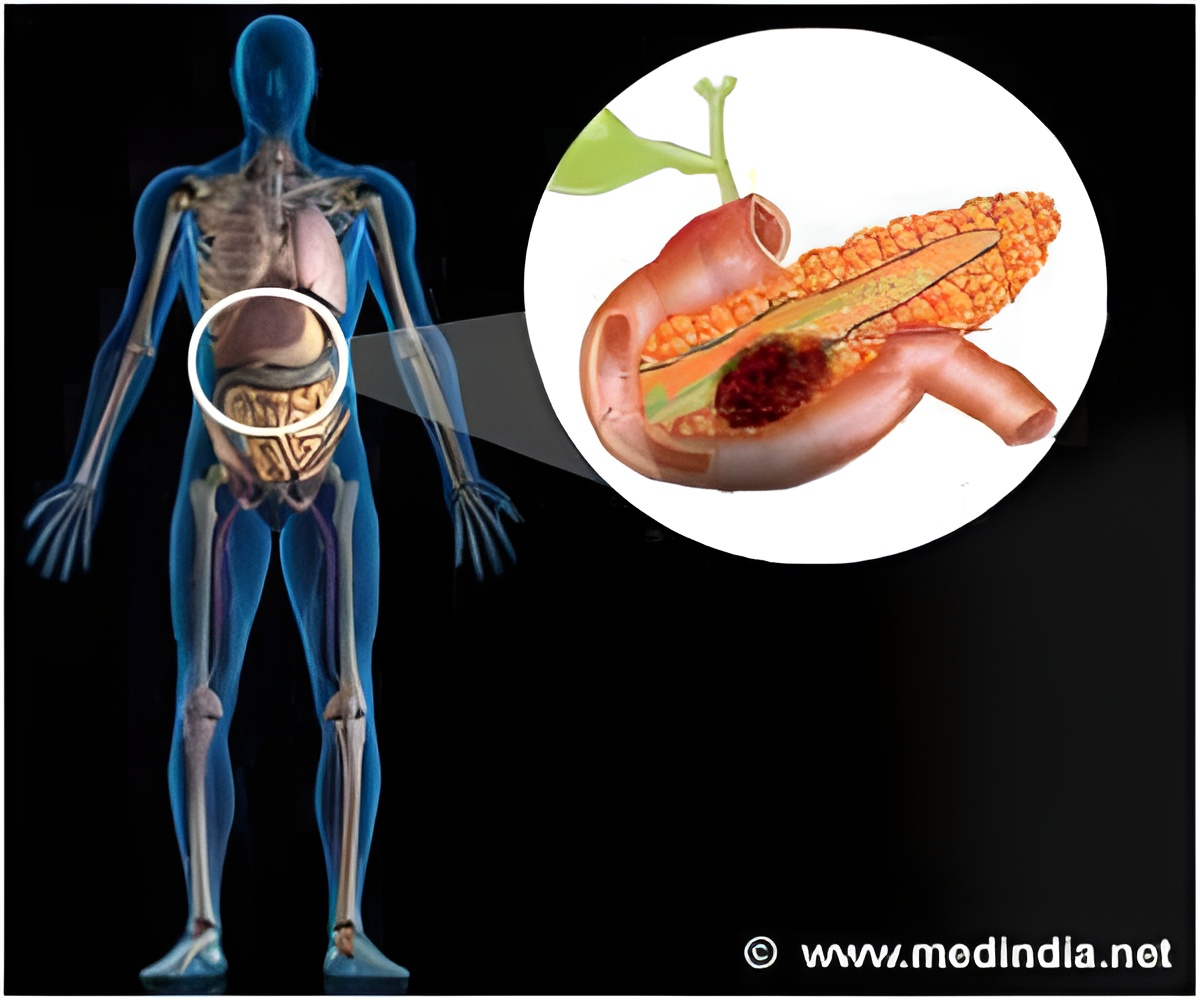
"It is the first example using induced pluripotent stem [iPS] cells to model cancer progression directly from a solid tumor, and the first human cell line that can model pancreatic cancer progression from early to invasive stages," says Zaret, also the associate director of the Penn Institute for Regenerative Medicine. "We were able to predict the appearance of cellular features and protein markers in the intermediate stages of pancreatic cancer that are not evident in the terminal stages. This has given us new perspectives into what this deadly type of cancer looks like – something no one has seen before in human cells.
Our analysis revealed known molecular networks that are activated during PDAC progression, as well as a new molecular network that is activated during the intermediate stages. This could provide a fresh outlook on biomarkers for early stages of the disease."A Leap of Faith Zaret and first author Jungsun Kim, PhD, a postdoctoral associate in the Zaret lab, hypothesized that if human PDAC cells were reprogrammed back to pluripotent cells and then allowed to re-differentiate into pancreatic tissue, they might undergo the early stages of cancer. To do this, they created the PDAC pluripotent cells and indeed found that they recapitulated the early to intermediate stages of pancreatic cancer.
They then isolated the cells at the early stage, cultured the cells in vitro, and identified the secreted and released proteins that might serve as early-stage biomarkers of disease progression. There's one caveat, though, says Zaret. "Using the iPS method, we could only get a cancer cell line from one patient to reprogram, meaning this work is representative of one individual's cancer," noting that his close collaboration with John Hoffman, a surgeon from the Fox Chase Cancer Center (FCCC) was key in order to get fresh cancer cells for the reprogramming. They tried this method with cells from nine human tumors in total.
However, as Zaret points out, there are many examples of where a single human cell line has served as a highly useful model for human disease. "Our iPS-like cells exhibited pluripotency, like other stem cells, but when they differentiated after we injected them into the immunodeficient mice, they preferentially developed into early-stage pancreatic cancer cells," says Zaret. He explains that the approach is another example of using iPS cells from human patients to model disease, by capturing the genome of an affected individual.
However, this is a first in solid tumor cancers, whereas many other labs have developed these types of cell lines for neurological and cardiovascular disorders.
Advertisement