Flexible sigmoidoscopy (FSG) ups the detection of colorectal cancer in women by one-fourth and in men by one-third, reveals study published in the Journal of the National Cancer Institute.

Using data from the PLCO cancer screening trial, Joel L. Weissfeld, M.D., MPH, associate professor in the department of epidemiology at the University of Pittsburgh, and colleagues analyzed results from participants aged 55-74 with FSG at study entry and then followed up with screening at 3 years and 5 years. Participants were enrolled in the study from 1993-2001. Persons who reported prior history of colorectal cancer or who had reported any lower gastrointestinal procedure conducted within 3 years of the study were excluded from participating in the study.
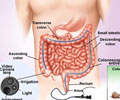
Of the 77,447 people enrolled in the study, 67,073 had at least one FSG and 39,442 had two FSGs. The researchers found that the second FSG increased the number of detected cancers or advanced adenoma by 26% in women and by 34% in men. Colorectal cancer or advanced adenomas were found in 3.8% of persons after the first screen and in 4.5% of persons after both screens, amounting to an increase in yield of 32%. Despite these findings, the researchers point out: "Although repeated FSG increases screening yields, it also increases the costs of screening, the need for diagnostic intervention, and the risks of complication." The researchers also point out the study's limitation, namely that this analysis does not include colorectal cancer mortality data because the data are not currently available. "Despite our ability to measure the yields from first and repeat FSG, it may not be possible to distinguish specific mortality benefits derived from first as opposed to repeat FSG."
In an accompanying editorial, Noel S. Weiss, M.D., DrPH, and Polly A. Newcomb, Ph.D., of the department of epidemiology in the School of Public Health at the University of Washington, write that it's important as well to look at previous studies in order to estimate the frequency of rescreening that will prevent the occurrence of clinically important cancers, and not just occult lesions (ie, small spots of pre-cancer that may never become full-blown cancer). They say that while those earlier studies focus on a clinically relevant endpoint, they nonetheless have potential limitations in regards to an appropriate screening interval. "A screening interval determined by the period between a negative screening exam and the clinical diagnosis may be longer than the one that could best achieve a reduction in cancer mortality," they write. Therefore, data from a study such as that of Weissfeld et al, with its identification of screen-detected pathology, are welcome. "The very large size of the study, and consequently the large number of cancer (26) and advanced adenomas (503) identified, provide statistically solid estimates for us to incorporate in cost-benefit evaluations of different rescreening strategies." However, the editorialists conclude that the limitations of all such studies (including that of Weissfeld et al) need to be taken into account when interpreting the existing data.
Source-Eurekalert