Researchers have successfully established the foundation for using hematopoietic (blood-producing) stem cells (HSC) from the bone marrow of patients with sickle cell disease (SCD) to treat the disease.
Kohn introduced an anti-sickling gene into the HSC to capitalize on the self-renewing potential of stem cells and create a continual source of healthy red blood cells that do not sickle. The breakthrough gene therapy technique for sickle cell disease is scheduled to begin clinical trials by early 2014. The study was published online ahead of press today in Journal of Clinical Investigation.
Gene Therapy
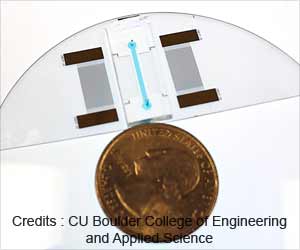
Kohn's gene therapy approach using HSC from patient's own blood is a revolutionary alternative to current SCD treatments as it creates a self-renewing normal blood cell by inserting a gene that has anti-sickling properties into HSC. This approach also does not rely on the identification of a matched donor, thus avoiding the risk of rejection of donor cells. The anti-sickling HSC will be transplanted back into the patient's bone marrow and multiplies the corrected cells that make red blood cells without sickling.
"The results demonstrate that our technique of lentiviral transduction is capable of efficient transfer and consistent expression of an effective anti-sickling beta-globin gene in human SCD bone marrow progenitor cells, which improved the physiologic parameters of the resulting red blood cells." Kohn said.
Kohn and colleagues found that in the laboratory the HSC produced new non-sickled blood cells at a rate sufficient for significant clinical improvement for patients. The new blood cells survive longer than sickled cells, which could also improve treatment outcomes. The success of this technique will allow Kohn to begin clinical trials in patients with SCD by early next year.
Sickle Cell Disease
Affecting more than 90,000 patients in the US, SCD mostly affects people of Sub-Saharan African descent. It is caused by an inherited mutation in the beta-globin gene that makes red blood cells change from their normal shape, which is round and pliable (like a plastic bag filled with corn oil), into a rigid sickle-shaped cell (like a corn flake). Normal red blood cells are able to pass easily through the tiniest blood vessels, called capillaries, carrying oxygen to organs such as the lungs, liver and kidneys. But due to their rigid structure, sickled blood cells get stuck in the capillaries and deprive the organs of oxygen, which causes organ dysfunction and failure.
Advertisement
CIRM Disease Team Program
This study was supported in part by a Disease Team I Award from the California Institute for Regenerative Medicine (CIRM), the state's stem cell research agency created by voter initiative in 2004. The purpose of the disease team program is to support research focused on one particular disease that leads to the filing of an investigational new drug application with the FDA within four years. The program is designed to encourage translational research, which means to take scientific discoveries from the laboratory to the patient bedside as quickly as possible. This requires new levels of collaboration between basic laboratory scientists, medical clinicians, biotechnology experts and pharmacology experts, to name a few.
Other support came from the UCLA Broad Stem Cell Research Center and Jonsson Comprehensive Cancer Center and the Ruth L. Kirschstein National Research Service Award.
Advertisement
Source-Newswise