Researchers used blood platelets and bone marrow cells to deliver potentially curative gene therapy to mouse models of the human genetic disorder Hurler syndrome.

Researchers were able to genetically insert into the cells a gene that produces a critical lysosomal enzyme (called IDUA) and then inject the engineered cells into mice to treat the disorder. Follow up tests showed the treatment resulted in a complete metabolic correction of the disease, according to the authors.
"Our findings demonstrate a unique and somewhat surprising delivery pathway for lysosomal enzymes," said Dao Pan, PhD, corresponding author and researcher in the Division of Experimental Hematology and Cancer Biology at Cincinnati Children's. "We show proof of concept that platelets and megakaryocytes are capable of generating and storing fully functional lysosomal enzymes, which can lead to their targeted and efficient delivery to vital tissues where they are needed."
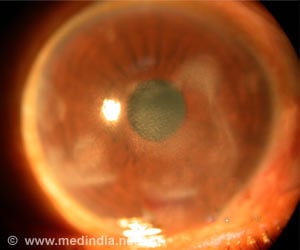
The mice tested in the study modeled human Hurler syndrome, a subset of disease known as mucopolysaccharidosis type I (MPS I), one of the most common types of lysosomal storage diseases. MPS I is a lysosomal storage disease in which people do not make an enzyme called lysosomal alpha-L-iduronidase (IDUA).
IDUA helps break down sugar molecules found throughout the body, often in mucus and fluids around joints, according to the National Library of Medicine/National Institutes of Health. Without IDUA, sugar molecules build up and cause organ damage. Depending on severity, the syndrome can also cause deafness, abnormal bone growth, heart valve problems, joint disease, intellectual disabilities and death.
Enzyme replacement therapy can be used to treat the disease, but it is only temporary and not curative. Bone marrow transplant using hematopoietic stem cells also has been tested on some patients with mixed results. The transplant procedure can carry severe risks and does not always work.
Advertisement
The authors said tests showed that human megakaryocytic cells were capable of overexpressing IDUA, revealing their capacity for potential therapeutic benefit. While engineering megakaryocytes and platelets for infusion into their mouse models of Hurler, the scientists report they were able to release IDUA directly into amply sized extracellular spaces or inside micro-particles as the cells matured or activated. The cells were able to produce and package large amounts of functional IDUA and retained the capacity to cross-correct patient cells.
Researchers cautioned that study results involving laboratory mouse models do not always translate into clinical treatment of human patients, and that additional research is needed for this prospective therapy.
Source-Eurekalert