Common genetic fusion TMPRSS2-ERG and interstitial gene retention may help identify patient’s risk of spreading prostate cancer.
‘Changes in the genetic events may identify prostate cancer patients at increased risk for disease progression from those whose risk of progression is low
’





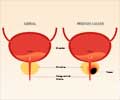
Different areas of a tumor may have different patterns, and the two highest patterns are added together to give the Gleason score. Most prostate cancers are Gleason score 6 (composed entirely of pattern 3) and men with Gleason score six are considered at low risk of having their tumors progress. Cheville explained that active surveillance is a common approach to caring for patients with prostate cancer with a Gleason score of 6. Men on active surveillance receive no treatment and are followed. Some of these men are later found to have the clinically significant disease that requires treatment.
Identifying a biomarker that, in addition to Gleason score, distinguishes men at increased risk for disease progression from those whose prostate cancer never becomes a clinically significant problem could help improve patient care, added Cheville.
To look for genetic biomarkers of clinically significant or insignificant disease, Cheville and colleagues used whole-genome mate-pair sequencing to study gene fusions in prostate cancer tissue samples obtained from 133 patients who underwent a radical prostatectomy at the Mayo Clinic.
The prostate cancers were divided into four groups: 53 low volume Gleason 6 tumors were classed as very low risk for progression; 26 high volume Gleason 6 tumors were classed as low risk for progression; 29 Gleason 7 tumors were classed as intermediate risk for progression, and 25 Gleason 8 or higher tumors were classed as high risk for progression.
Advertisement
Among the 60 prostate cancers with TMPRSS2-ERG fusions, 39 had deleted the interstitial genes between TMPRSS2 and ERG during the fusion event, and 21 had retained these genes. Eighteen of the 21 prostate cancers that had retained the interstitial genes during TMPRSS2-ERG gene fusion was in the very-low-risk and low-risk groups.
Advertisement
In univariate, but not multivariate, analysis, biochemical recurrence was significantly lower if the prostate cancer had a TMPRSS2-ERG gene fusion with interstitial gene retention compared with those that had interstitial gene deletion.
Author Comment: "Our data support results from other studies in that the presence or absence of a TMPRSS2-ERG gene fusion was not predictive of outcome," Cheville said.
"But how the gene fusion formed was important; the retention of interstitial genes during the fusion event was more common in very-low risk and low-risk cancers, and there may be genes in this region that suppress or limit tumor growth.
There is the potential utility for determining the status of interstitial genes in stratifying men with prostate cancer into more well-defined risk groups, but this will require further study before it can be incorporated into clinical practice.
"The loss or retention of interstitial genes was tied closely to Gleason score, and we did not have enough cases to determine whether or not the type of fusion was an independent marker for biochemical recurrence," continued Cheville.
"We need to look at many more samples and also look at patients with higher Gleason scores to determine the extent to which loss of interstitial genes is associated with disease progression."
According to Cheville, the main limitation of the study is the relatively small number of patients analyzed in each group.
This study was supported by James and Dorothy Nelson Benefactor Funds and the Mayo Clinic Center for Individualized Medicine. Cheville declares no conflicts of interest.
Source-Eurekalert