Blood cancers in pregnancy pose unique challenges, with no established clinical guidelines for care.
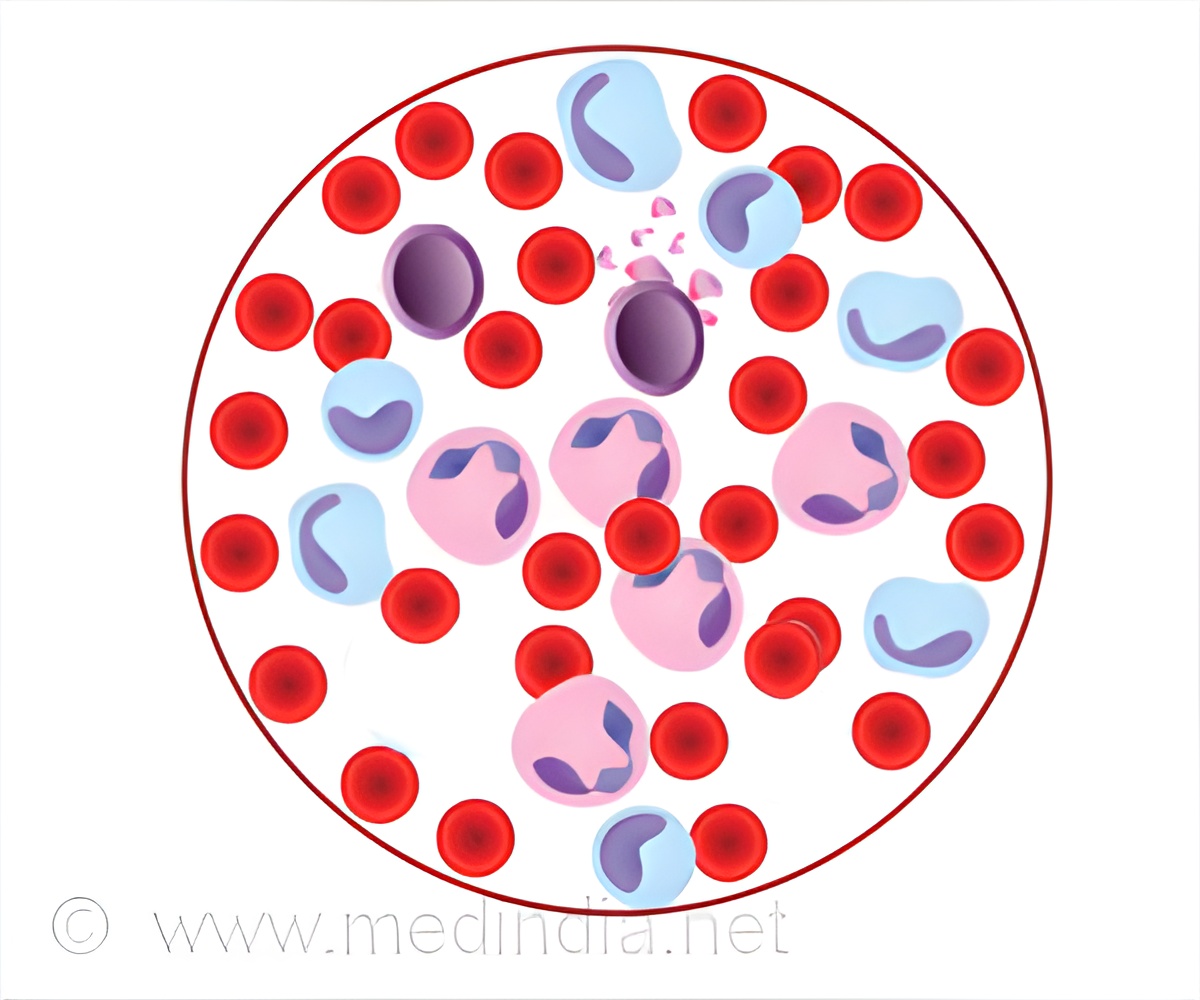
‘Around 12.5 #pregnancies per 100,000 are affected by #bloodcancers like #leukemia and #lymphoma? And the numbers are rising.’





An Australian working group has now published a new position statement in the latest edition of The Lancet Haematology, based on current evidence and expert consensus.It forms a practical guide for doctors, including recommendations for diagnosis and staging, imaging safety in pregnancy, therapy in pregnancy incorporating a multidisciplinary approach, supportive care, oncofertility, and pregnancy and birth management.
Challenges Faced by Pregnant Women with Cancer
Lead author Dr. Georgia Mills from Macquarie Medical School says a cancer diagnosis in pregnancy is incredibly distressing for a patient and her family.“But on top of this, women can experience treatment delays, inaccurate information and communication breakdowns, all of which increases the worry associated with a cancer diagnosis and fears for their unborn baby,” she says.
“Patients have also described a lack of sensitivity about fertility preservation, breastfeeding, medication risks to the unborn baby, and a lack of information and support groups.
Advertisement
Senior author Dr. Gisele Kidson-Gerber says taking a multidisciplinary approach was of paramount importance in preparing the guidelines.
“Most treatments are possible during pregnancy, including many forms of chemotherapy, but this is not what patients expect.”
The guidelines were drafted using co-design principles, with a patient representative on the working group to ensure patient concerns were well understood.
Victoria Bilsland was diagnosed with stage 4B nodular-predominant Hodgkins lymphoma when she was 17 weeks pregnant.
But with her symptoms repeatedly dismissed as pregnancy pain or possible infection, just getting a diagnosis was a struggle that led her to lose faith in doctors.
“I was told I ‘needed spinal surgery’ and to ‘consider termination’, and when I declined termination as we still didn’t know the extent of the cancer, I was advised to ‘think logically’,” she says.
“I was offered to terminate my pregnancy on multiple occasions, but I had no information about the risks to me or my baby, or knowledge of what stage the cancer was or even where it was.
“How could I make an impossible decision without information? And why could no one provide me information regarding cancer and pregnancy?
“The process was a rollercoaster of trauma, depression and anxiety.”
Eventually put into the care of a specialist team experienced in managing haematological cancers in pregnancy, she received appropriate treatment and delivered a healthy son at 32 weeks.
She hopes the new guidelines will help other doctors to make the same decision in a timely way, putting the patient first and reducing potential trauma.
The guidelines have been endorsed by the councils of the Society of Obstetric Medicine of Australia and New Zealand and the Haematology Society of Australia and New Zealand.
Source-Eurekalert