Scientists have developed a method that could result in the development of capillaries in tissues using a semisynthetic medium of gelatin methacrylate.
- The development of tissues in the laboratory could solve the problem of tissue availability for transplantation
- Scientists have found it difficult to develop tiny blood vessels called capillaries to nourish such tissues
- A new method suggested and tested by scientists could possibly overcome this problem
Any tissue that is a few cells thick requires the presence of tiny blood vessels called capillaries to provide nutrition and oxygen to the cells, and to remove carbon dioxide and waste products out of them. Capillaries arise from small arteries called arterioles, form a network within tissues and drain into small veins called venules. Therefore, tissue that is engineered in the laboratory requires the presence of capillaries, without which they cannot survive.
The capillaries are very thin walled, and contain a single layer of cells called the endothelial cells. This is in contrast to the arteries and the veins, which also contain a muscle layer surrounding the endothelial layer; the muscle layer is thicker in the arteries as compared to the veins. The muscle layer is surrounded by another layer consisting mainly of collagen.
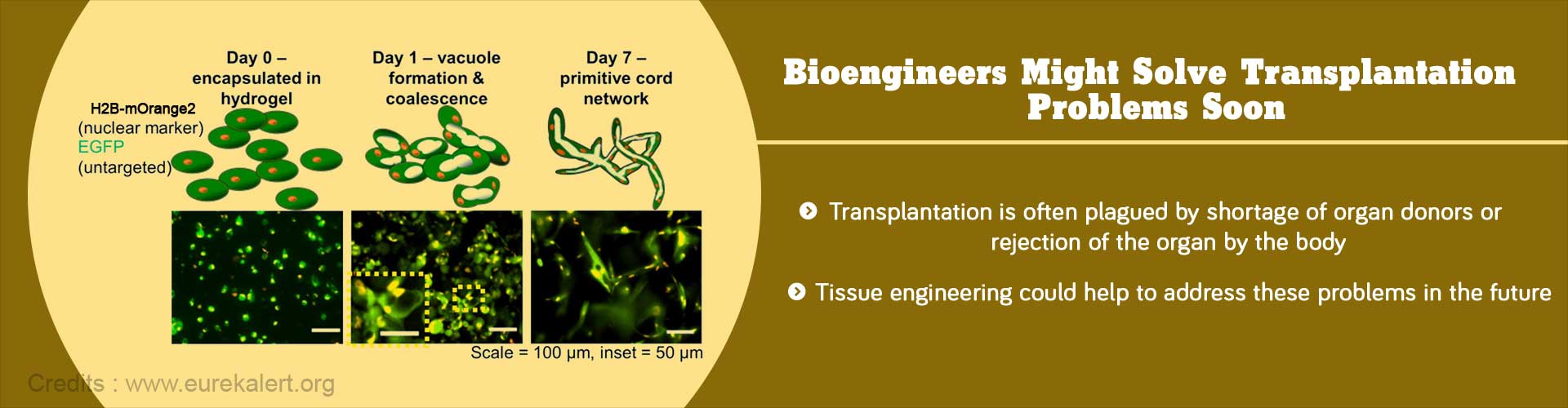
When capillaries develop, they undergo a process called tubulogenesis, in which they assume the tubular shape of a blood vessel. The cells develop vacuoles that join together, leading to the formation of a tubular network through which blood can pass. This process is difficult to replicate in the laboratory.
Through their experiments, scientists found that it may now be possible to produce capillaries in the laboratory.
- They used induced pluripotent stem cells (iPSCs) to produce the endothelial cells of the capillaries. iPSCs can be produced from any adult, and are therefore specific for the patient. This could probably solve the problem of tissue rejection.
- They modified the cells to produce two types of fluorescent proteins, one in the nucleus and the other throughout the cell. With the help of these, they could study the cells under the microscope and monitor the changes going on in the cells.
- The cells were then mixed with fibrin, which is a natural medium, with or without another type of cell called the mesenchymal stem cells. They were incubated for a week. This procedure resulted in good tubulogenesis, irrespective of the presence or absence of the mesenchymal cells.
- Tubulogenesis was more difficult when the cells were incubated in a semisynthetic medium called gelatin methacrylate. This difficulty was overcome by the addition of mesenchymal stem cells. This finding is important since gelatin methacrylate has a great potential to be used for tissue engineering.
Reference:
- Calderon GA et al. Tubulogenesis of co-cultured human iPS-derived endothelial cells and human mesenchymal stem cells in fibrin and gelatin methacrylate gels. Biomater. Sci., (2017), Advance Article. DOI: 10.1039/C7BM00223H