Skin grafting attempts to reduce wound appearance. Read on to find out more about how skin grafting can help restore wellness among patients that have undergone extensive injuries and/or burns.
Skin grafting is a surgical procedure wherein the skin from one part of the body is removed or peeled, and transplanted to another part of the body. The transplanted part is known as the ‘skin graft’. Also known as skin auto grafting, skin transplant, full thickness skin graft and split thickness skin graft, this surgery is carried out when a patient has suffered from burns, a skin infection or ulcer, or has undergone a surgery for skin cancer.
Accident survivors with large wounds that cannot be closed even by a surgeon may also require to undergo this procedure. Also, diabetic patients having non-healing ulcers can benefit from this surgery.
The procedure
The surgical procedure is carried out under general anesthesia as it can be quite painful. To extract the skin graft from a healthy area, the surgeon uses an instrument called ‘dermatome’. This instrument removes the epidermis and a part of the dermis from the healthy skin, leaving behind hair follicles and a few epidermal cells on the skin, which proliferate and heal within a few days. This area can be quite painful and is extremely susceptible to infections.
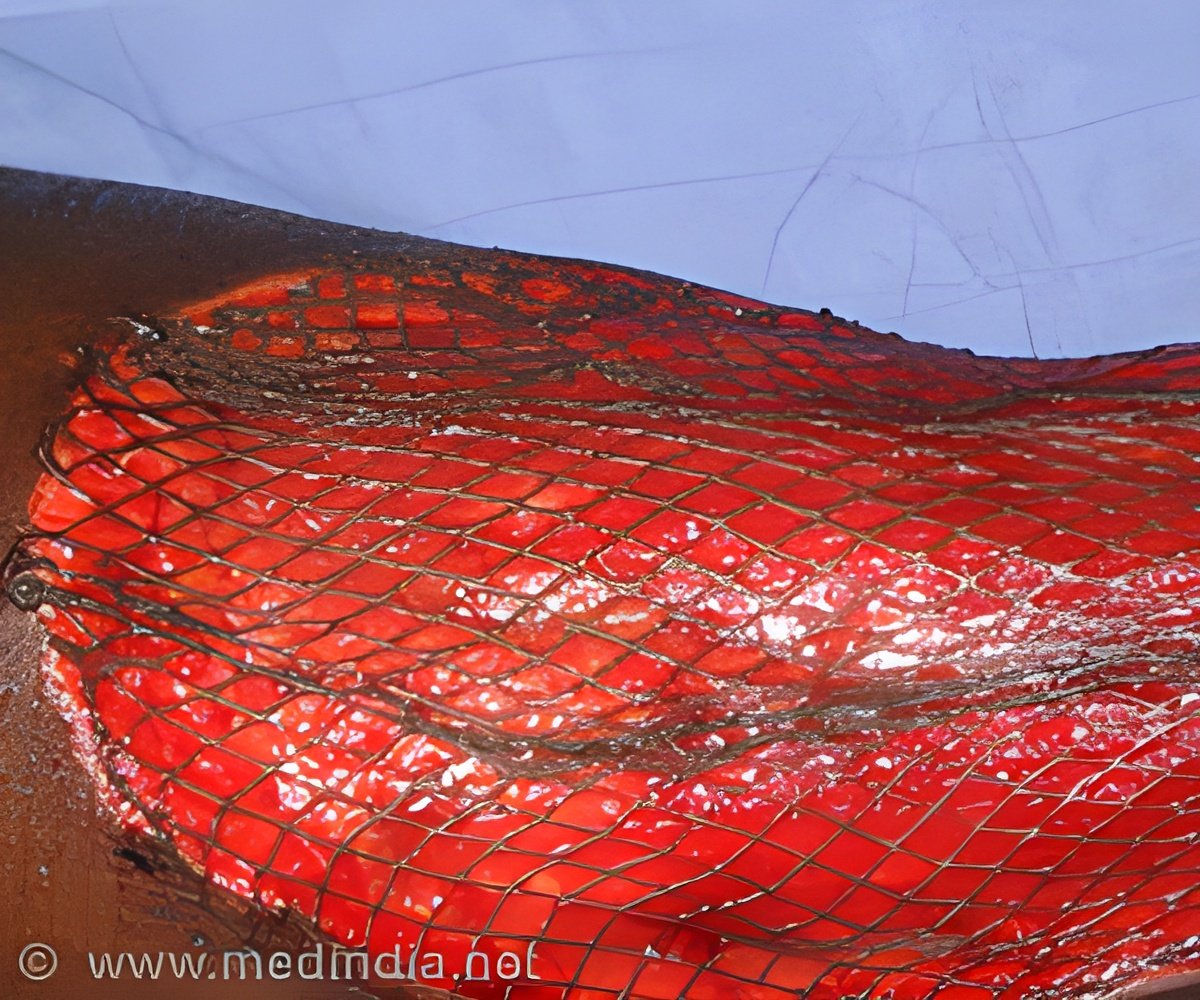
The skin graft is then placed over the required area and held in place by staples, stitches or heavy dressings. It is then nourished by allowing it to imbibe plasma and encourage blood vessel formation, promoting speedy healing.
Allograft: Removal of healthy tissue from the patient itself is known as an allograft.
Auto graft: Auto graft involves the removal of the skin graft from the patient itself. This grafting requires a good amount of physical strength from the patient and cannot be performed on patients who have recently undergone traumatic accidents or burns. Use of auto grafts demonstrates minimal tissue rejection.
Isograft: Skin graft obtained from a monozygotic twin is known as an Isograft.
Prosthetic graft: Prosthetic grafts make use of metals, ceramic, or other synthetic materials to replace the lost tissue.
Split thickness graft: In cases of shallow wounds or minor burns, split thickness grafts are used. They involve the extraction of epidermis and a part of the dermal tissue only.
Full thickness graft: Full thickness grafts are used in case of major burns and extensive injuries. They require extraction of the epidermis, dermis and the hypodermis from the donor.
Composite graft: Wounds that include bone, muscle and/or tendons require composite grafts. Nose reconstruction surgery is a good example of a composite graft.
Possible complications
Since the donor area is exposed and has lost the protective layer of the skin (epidermis), it becomes highly susceptible to infections. Bleeding and nerve damage have also been observed among 13% patients that have undergone this surgical procedure. In cases when the skin graft is not extracted from the patient itself (xenograft), rejection may occur, which may need to be treated by immunosuppressant drugs.
Other complications include loss of skin sensation or increased sensitivity, chronic pain, reaction to medications and breathing problems. Irregular tissue, scarring and discoloration of skin make it look less aesthetically appealing.
Artificial skin grafts
There is not enough healthy donor skin available for patients who have suffered 80-90% burns. Research on artificial skin development is being conducted since the late 1970’s and finally, the introduction of ‘Integra’ a new artificial skin design has proved to be a boon to patients suffering 2nd and 3rd degree burns.
Integra doesn’t replicate the function of healthy skin; in fact, it tricks the skin to grow back in a manner similar to normal wound recovery process by stimulating fibroblasts to generate collagen fibers. It acts as a stimulator and can be peeled of the skin once the dermis is fully grown.
Source-Medindia















