A technique using bag-mask ventilation during tracheal intubation helps patients breathe better and could potentially save lives. This technique helps patients’ breathe during dangerous procedures and prevents complications.
- Using bag-mask ventilation during tracheal intubation will help patients breathe better
- Using the device will prevent complications and could potentially save lives
- The results of a new study have the potential to change practice across the U.S
A new study from the Vanderbilt University Medical Center (VUMC), featured in the New England Journal of Medicine (NEJM) has shown that using bag-mask ventilation to squeeze air from a bag into the mouth of a patient for 60 seconds will help in breathing, improve outcomes and could also potentially save lives.
Read More..
Why is Ventilation Safe?
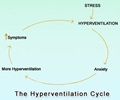
Jonathan D. Casey, MD, a Pulmonary and Critical Care Fellow at VUMC and the first author of the study said, “When you place a breathing tube, you have to give patients medications to make them relaxed and sleepy. And those medications take about a minute to kick in.”“After you give those medications, there is a big divide among doctors about whether to just wait and watch while their breathing slows and stops, or to provide ventilation (breath for the patient) with a bag-mask device. We found that providing ventilation with a bag-mask device is safe and very effective. Most importantly, it cut the rate of severely low oxygen levels in half,” added Dr. Casey.
The PreVent Trial
The PreVent trial (Preventing Hypoxemia with Manual Ventilation during Endotracheal Intubation) was a multicenter trial of using bag-mask ventilation during tracheal intubation. The results of the trial have been published in the NEJM. In a country like the U.S, where more than 1.5 million patients undergo tracheal intubation each year, the study results could potentially influence a change in practice across the entire nation.On why bag-mask ventilation is not being used commonly, Dr. Casey said, “Doctors have been performing this procedure for 50 years and there has always been controversy about the safest way to do it. Some doctors believe that when you squeeze the bag and force air into the lungs that will also put air into the stomach and put the patient at risk for vomiting of stomach contents into the lungs.”
“That is not what we found. Our study found that bag-mask ventilation didn't cause the vomiting that people were worried about, and it was very effective at preventing low oxygen levels,” added Dr. Casey, quoting the findings of the study.
The multicenter trial was conducted in seven ICUs throughout the U.S. Adult patients who were a part of the trial, underwent the procedure with one group receiving ventilation with a bag-mask device, while the other had no ventilation between induction and laryngoscopy.
Study Results
A total of 401 patients had enrolled in the trial. Among them, in the bag-mask ventilation group, the lowest median oxygen saturation was 96 percent, whereas, it was 93 percent in the no-ventilation group.While 45 patients had severely low oxygen levels in the no-ventilation group, only 21 patients in the bag-mask ventilation group were found to have low levels.
In the bag-mask ventilation group, there was vomiting of stomach contents into the lung in 2.5 percent of intubations, whereas in the no-ventilation group, it was as high as 4 percent.
Conclusion
Using bag-mask ventilation during placement of a breathing tube has now become a routine at the Medical ICU of Vanderbilt.The Associate Director of the Medical ICU at Vanderbilt and senior author of the study Matthew W. Semler remarked, “It is important to act on what we learn. Not only did we immediately apply these important results to our practice, but we have started follow-up trials of other ways to improve the safety of tracheal intubation - and those new trials require that bag-mask ventilation is provided for every patient receiving a breathing tube.”
In conclusion, “The best thing about this intervention is that it is free. This is a device that is already always available when you are placing a breathing tube. In the past, we only used the bag-mask device to assist patients' breathing if we had difficulty placing a breathing tube. Now we know that it should be used in every procedure even before we make our first attempt to place a breathing tube,” said David R. Janz, Assistant Professor of Medicine at Louisiana State University and a co-author on trial.
Reference:
- VUMC study finds that helping patients breathe during intubation prevents life-threatening complications - (http://news.vumc.org/2019/02/18/vumc-study-finds-helping-patients-breathe-during-intubation-prevents-life-threatening-complications/)
Source-Medindia