Which form of primary screening for cervical cancer should you opt for according to cost effectiveness and your age? Find out from this report.
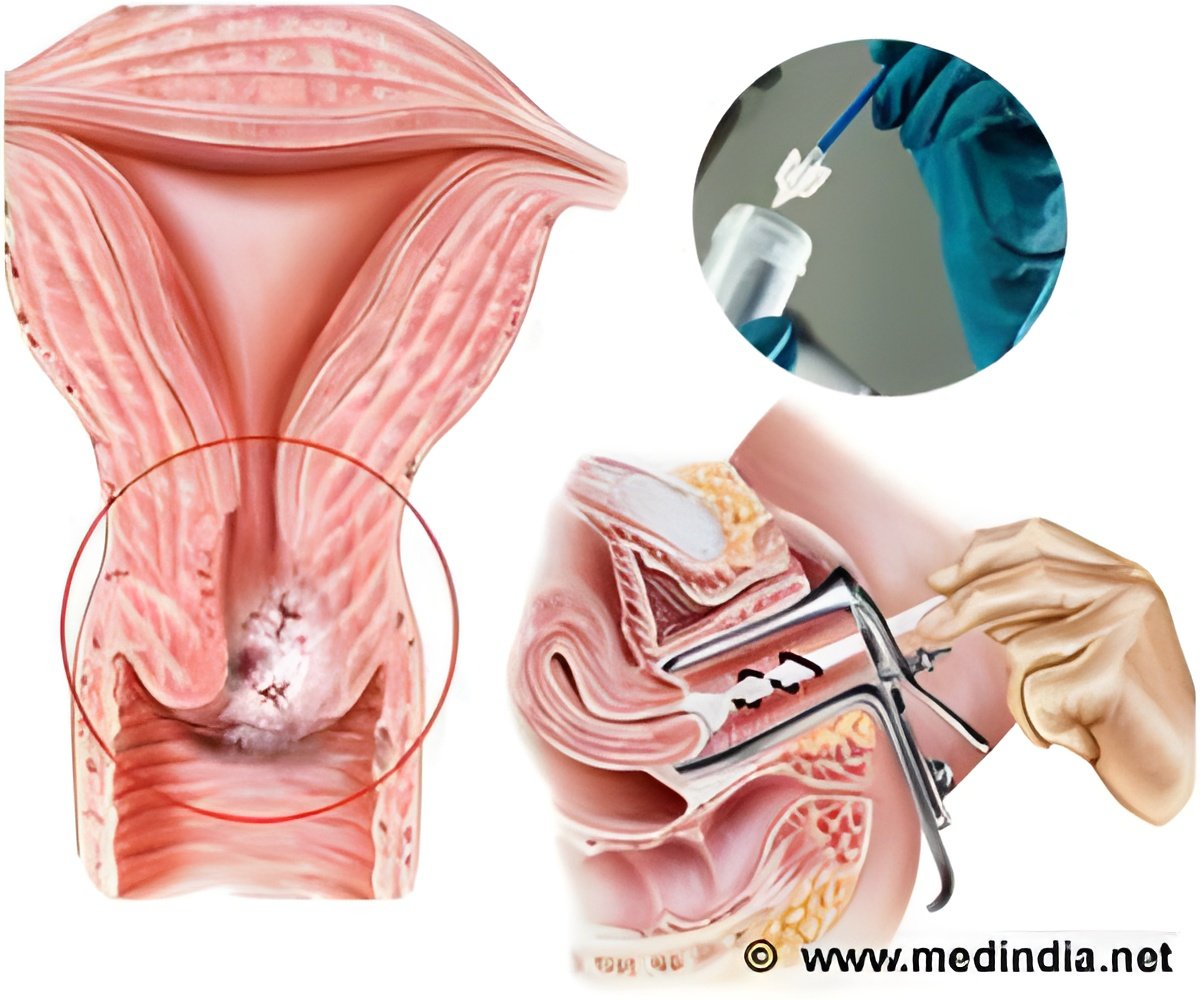
Cervical cancer starts with a pre-invasive stage called cervical intraepithelial neoplasia (CIN) or abnormalities in the epithelial cells of the uterus and is curable. It progresses slowly and reaches an invasive stage when it is very difficult or mostly incurable. Needless to say it becomes a very expensive treatment.
Screening for cervical cancer helps find the disease at an early stage when there are no symptoms thus allowing for better chance of cure. Screening is done basically either by HPV test (or screening for human papillomavirus) or in addition to a Papanicolaou test, commonly called the Pap smear, which can be conventional or liquid based.
In countries where cervical cancer screening is the primary preventive strategy, it is being debated whether or not to replace cytology screening with HPV screening. A Swedish study found that ‘incorporating HPV testing in primary cervical screening improves sensitivity and maintains a high positive predictive value, thus minimizing unnecessary referrals’.
However, comparison between HPV testing and cytology screening is not that straightforward. It depends on the quality of cytology screening and the prevalence of HPV infections relative to the level of risk for cervical cancer. The cost of screening is also an important criterion for comparison, especially in Europe. For example, the German statutory health insurance (SHI) funds reimburse HPV testing only when the result of a Pap smear is unclear.
So, Marjolein van Ballegooijen from Erasmus MC, University Medical Center, Rotterdam, Netherlands, and colleagues took up a study to investigate the ‘balance between benefits, burden, and costs of HPV screening compared with cytology screening for various scenarios based on combinations of variables observed in several European countries’ with the objective of finding out whether and under what variables screening for HPV is preferred over cytology screening for cervical cancer, from the cost effectiveness point of view.
- Risk of cervical cancer
- Previous screening
- Quality associated test characteristics
- Cost of testing
- Prevalence of HPV
Cost effectiveness analysis was based on a Dutch simulation model or the micro simulation screening analysis (MISCAN) model. This model simulates a large study population (unvaccinated women born between 1939 and 1992, in this case) in which women will acquire HPV infections, develop pre-invasive cervical lesion and get cervical cancer. Some may die from the cancer. Alternatively, infections can clear or the cancer can regress. Now, if this simulated population undergoes screening, there will be changes in the age specific and time specific output of disease incidence and mortality in terms of number of events and stages induced or prevented.
The MISCAN model produces the number of life years spent (QALY – quality adjusted life years) in each state as well as the number of certain events, such as screenings and cervical cancer diagnoses, in a woman’s lifetime.
The results showed that:
- Primary HPV screening was preferred over primary cytology screening in most of the scenarios except where in high HPV prevalence scenario and where the cost of screening was very high.
- Primary cytology screening was preferred in cases of higher costs for HPV screening and in high HPV prevalence scenario.
- Primary cytology was preferred, in the scenario with low costs for cytology, irrespective of lower sensitivity and specificity that accompanied the lower costs in some eastern European countries such as Romania, Bulgaria, the Slovac Republic and Latvia.
- Primary HPV screening was the preferred primary test over the age of 30 in many considered scenarios.
- In countries like the United Kingdom and Italy where population based primary HPV screening trials are not yet implemented, reliable estimates for the prevalence of HPV are often not available.
- It is not clear whether the situation of high prevalence of HPV and high costs for the HPV test is common in Europe.
‘It is important to organize primary HPV screening in such a manner that the costs of the test are low. This can be achieved by concentrating the large numbers of HPV DNA tests in large laboratories to achieve economy of scale effects, such that the costs per test are lower if more test are analyzed.’ – stated the authors.
Although the investigators did not consider strategies that differ by age group, they found that, from a cost effectiveness point of view, primary cytology screening is preferred under the age of 30.
Another limitation was not including men in their study model since men influence the prevalence of HPV in the female population, owing to sexual interaction. ‘Since HPV screening has a higher sensitivity, more HPV infection can in theory be removed from the population and the chance of becoming infected with HPV could be lower in the case of HPV screening,’ they say.
In conclusion, they recommended that European countries should switch from primary cytology to HPV screening. Also, they feel that it is important to organize primary HPV screening in such a way that the procedures are carried out in large centers to monitor the quality of the screening and to ensure that the costs of the test are low.
Reference: 1. de Kok IM, van Rosmalen J, Dillner J, Arbyn M, Sasieni P, Iftner T, van Ballegooijen M. Primary screening for human papillomavirus compared with cytology screening for cervical cancer in European settings: cost effectiveness analysis based on a Dutch microsimulation model. BMJ. 2012 Mar 5; 344:e670. doi: 10.1136/bmj.e670.
2. http://jnci.oxfordjournals.org/content/early/2009/01/13/jnci.djp003.full
Source-Medindia