Scientists discover why it is difficult to bring out mucus from the airways in certain lung diseases such as cystic fibrosis and chronic bronchitis by means of coughing.
- Scientists find out why coughing is unable to get rid of mucus secretions in lung conditions such as cystic fibrosis and chronic bronchitis
- The physical and chemical properties of normal mucus and mucus in disease states vary greatly and the increased strength and viscosity of mucus in lung diseases makes it difficult to be cleared out by coughing
- Treatments that reduce the strength and viscosity of mucus in lung diseases allow it to be more easily brought out by coughing
Read More..
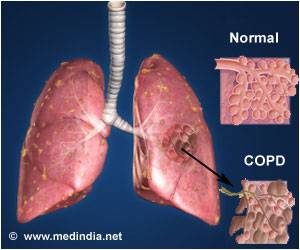
Typically, the cough reflex creates high-velocity airflow that breaks apart the mucus and simultaneously tears it free from the airway lining which then enables it to be coughed out. This process seems to be affected in lung conditions such as asthma, COPD, cystic fibrosis and chronic bronchitis.
- The team at UNC developed a sophisticated system to test the mechanical force needed to dislodge and break up normal as well as cystic fibrosis (CF) type mucus.
- They obtained airway-lining cells from the lungs of transplant patients and grew them in laboratory dishes. These cells were then able to produce their own mucus and appeared like miniature versions of actual airway lining cells
- Since, mucus is a soft sticky substance, the team developed a method to embed tiny meshes, which bind firmly to the mucus.
- Using a silk thread, this mesh was then connected to a motor having a force sensor to quantify the force required to tear apart the mucus from the lining of the airways
- This arrangement enabled testing of the adhesive and cohesive forces of mucus and comparing these forces in normal mucus and disease associated mucus.
Testing the Efficacy of Popular Cystic Fibrosis Treatments in Altering the Property of Mucus
The UNC and Duke scientists also used this experimental design at the same time, to test the efficacy of two popular forms of CF treatments on the properties mucus in cystic fibrosis.
- First treatment - inhaled saline and hypertonic saline (more salt content than body water) - increases the water content in mucus to make it thinner.
- Other types of treatments or "mucolytic" agents decrease viscoelasticity of mucus by cutting up or separating mucin molecules, thereby reducing the stiffness of the mucus
Senior author Michael Rubinstein, professor in the Department of Mechanical Engineering and Materials Science at Duke University, said, "We measured the adhesive forces that bind mucus to the airway lining and the cohesive forces that hold mucus together, and identified several agents that show promise in reducing the strength of mucus's adhesive and cohesive interactions."
For most patients and for minor respiratory ailments, either of these therapies will work, but since their effects are additive, combining the two treatments will be of benefit in patients with severe airway diseases.
To use the experimental system, it is necessary to study in detail the properties of mucus and response to therapies in other respiratory diseases as well and see how mucus clearance can be improved with newer strategies.
- Can Scientists Change Mucus to Make It Easier to Clear, Limiting Harm to Lungs? - (http://news.unchealthcare.org/news/2018/november/can-scientists-change-mucus-to-make-it-easier-to-clear-limiting-harm-to-lungs)
Source-Medindia