Questions have been raised about the continued use of the dengue vaccine due to increased risk of severe infection in persons previously unexposed to the virus.
- Emerging data suggests that the dengue vaccine increases the risk of severe disease and hospitalization due to dengue infection in individuals who were not previously exposed to the virus.
- The infection is not caused by the vaccine per se, but by reinfection by a dengue virus from the environment.
- The issue could be resolved by testing individuals for prior infection before the administration of the vaccine.
The reason for this unexpected adverse effect can be explained based on the way the body reacts to a natural dengue infection. Dengue infection is caused by four subtypes or serotypes of the virus. An infection with one serotype provides life-long immunity against the specific type of dengue virus, but a second infection by a different serotype can occur and often results in a serious disease. A third or fourth infection, however, is usually mild.
It is therefore suggested that a similar reaction occurs with vaccination as well. If the individual was never exposed to the virus earlier, the vaccine acts as the first or primary infection. A subsequent natural infection thus becomes a second infection and is more likely to be severe. However, if the individual was previously exposed to the virus, the vaccine acts as a second infection, which cannot be severe since the virus is inactivated in the vaccine. Thus, a future natural infection acts as the third or fourth infection, which is again mild.
One of the reasons why the dengue vaccine was not approved for use in children younger than 9 years was that clinical trials revealed an increased chance of hospital admission for dengue in children between 2 and 5 years in the third year following the administration of the vaccine. It is possible that the younger children were not exposed to the virus earlier. The vaccine therefore acted as a primary infection and a subsequent natural second infection was more likely to be severe.
In view of the above, blood tests were carried out by the manufacturer on samples obtained from vaccinated individuals to find whether the individuals were exposed to dengue infection before the vaccination. They concluded that:
- The vaccine protected people who were exposed to the dengue virus before the vaccination, against severe dengue infection and hospitalization for 5 years
- People who were not exposed to the dengue virus before the vaccination were more likely to suffer from serious dengue infection following the vaccination. The risk was highest in the third year following the first dose of the vaccine
The World Health Organization (WHO) has recommended that vaccine should be administered only to individuals who were earlier infected with dengue. Several individuals, however, may have had an asymptomatic disease or a mild disease that could have be mistaken for any other viral infection, and may not even know that they had a previous infection.
Currently, the WHO advises the use of the vaccine only in those who have a proven infection, either by a diagnostic test or a previous documented medical history of an infection. The WHO is expected to review and re-state its stand on the use of dengue vaccine in April 2018. The publication will hopefully provide more clarity on the issue.
About Dengue
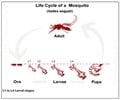
Dengue is a viral infection spread through the bite of the Aedes mosquito. The virus exists as 4 different serotypes. While majority of the cases result in mild illness and respond to symptomatic treatment, sudden death due to complications like bleeding and shock are not uncommon. Currently, no definite treatment for dengue exists. Platelet transfusion and fluid infusion has been life-saving in several cases. There is some emerging evidence about the protective effects of papaya leaf extract to improve platelet counts in dengue patients. Prevention from dengue is mainly directed at preventing mosquito bites.References:
- The dengue vaccine dilemma. The Lancet Infectious Diseases 2018: 18(2):123. DOI: http://dx.doi.org/10.1016/S1473-3099(18)30023-9
- Updated Questions and Answers related to the dengue vaccine Dengvaxia® and its use - (http://www.who.int/immunization/diseases/dengue/q_and_a_dengue_vaccine
_dengvaxia_use/en/)