Wilson's disease must be considered in anyone whose presenting symptoms include a combination of unexplained liver disease and neurological or neuropsychiatric disorders.
When this function is impaired due to a genetic abnormality, there is an accumulation of copper in the body, including the vital organs such as the liver and the brain. The disease is fatal if left untreated.
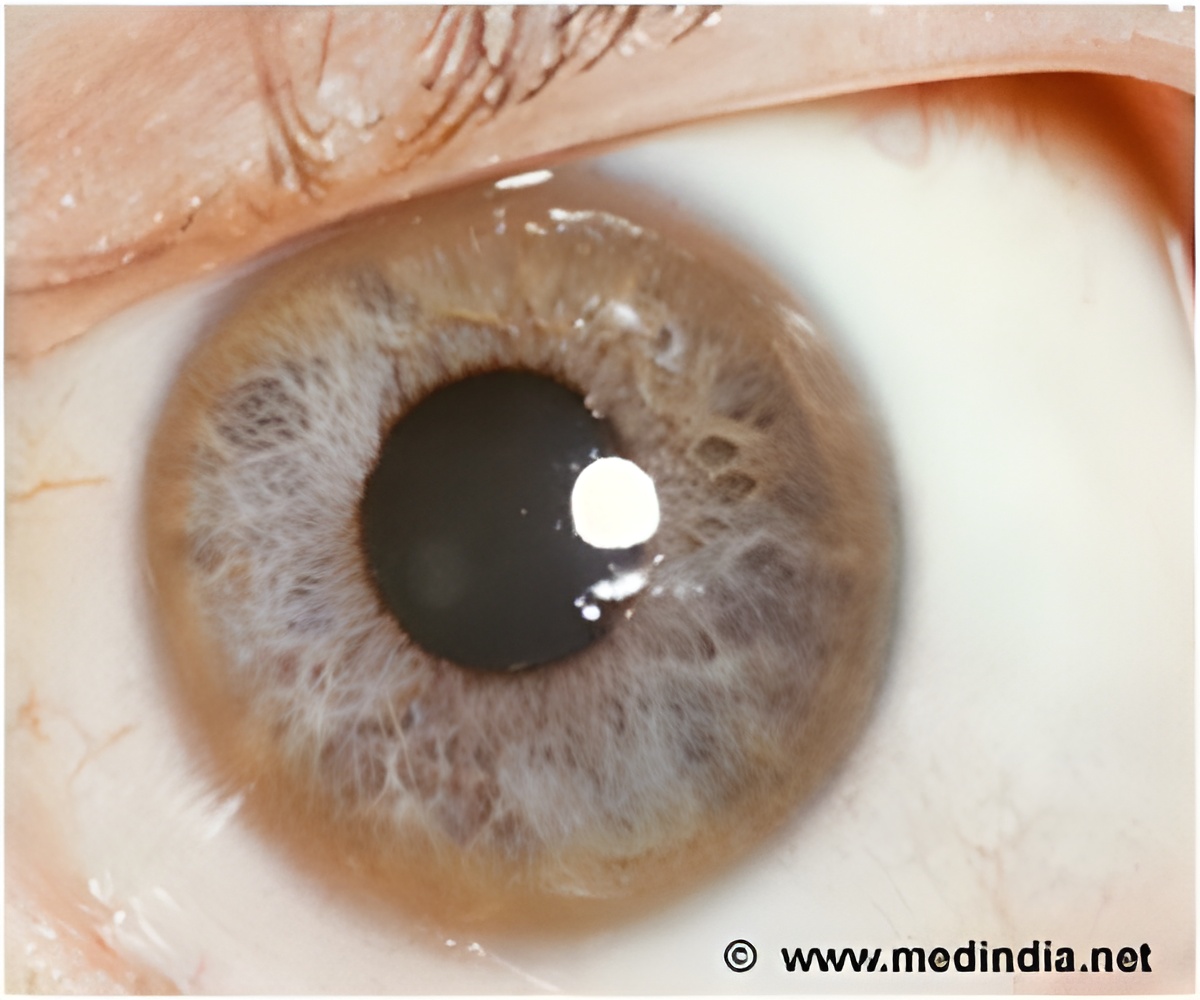
The first European Clinical Practice Guidelines (CPGs) for the effective diagnosis and management of Wilson's disease were published recently by the European Association for the Study of the Liver (EASL). Lead author Professor Peter Ferenci said: "The clinical presentation of Wilson’s disease can vary widely, but it must be considered in any patient who presents with a combination of unexplained liver disease and neurological or neuropsychiatric disorders. In the absence of Kayser-Fleischer rings which are typical but not always present, the guidelines recommend measurement of urinary copper excretion and hepatic parenchymal copper as diagnostic methods of choice. Notably, age alone should not be the basis for eliminating a diagnosis of Wilson's disease."
Professor Roderick Houwen added: "Unfortunately, as there are no optimally designed randomized controlled trials conducted in Wilson’s disease, there is a lack of high-quality evidence to estimate the relative treatment effects of the available drugs. Our evaluation is mostly based on large case series that have been reported in recent decades, which highlights a clear need to conduct more robust randomized controlled trials to better understand treatment for this rare condition."
Symptoms & Signs
a) Physical signs of Wilson’s disease include the Kayser-Fleischer rings, which are present in the majority but not all of WD patients. These rings are caused by the deposition of copper in the cornea of the eye and can be detected by slit-lamp examination by an expert. These rings are not exclusive to WD but can also be found in other conditions as well.
c) Neurologic disease - Those with Wilson’s disease may present with neurologic, psychologic or behavioral disorders. These may be presenting symptoms or may manifest years later. The neurologic symptoms include coarse tremors, abnormal muscle tone and difficulty with balancing. - Facial grimacing, open mouth, drooling, lip retraction and speech changes are some of the common manifestations. The patient may have more than one of these symptoms with varying degrees of severity. Eventually the WD patients with neurologic symptoms become bed-ridden due to severe disability, although they manage to remain alert. Behavioral and psychological symptoms are very common and tend to precede the neurologic symptoms.
Diagnosis
A combination of Kayser-Fleischer rings along with low levels of serum ceruloplasmin are sufficient to diagnose Wilson’s disease.
Tests are carried out to confirm the diagnosis are:
• Ceruloplasmin levels - Ceruloplasmin is a most important copper carrying compound present in the blood. It is typically low in patients with neurologic Wilson’s disease, but it can be on the lower normal range in those WD patients with liver problems.
• 24 hr urinary copper - Determining the amount of copper excreted through urine is extremely important in diagnosing Wilson’s disease. In a symptomatic patient who is untreated, the baseline copper excretion that is greater than 1.6 micromol/24hrs is considered as a sign of Wilson’s disease. However, this value is less in affected children and in their asymptomatic siblings. In children, urinary copper excretion greater than 0.64 micromol/24 hours can be considered suggestive of Wilson’s disease.
• Hepatic copper - Estimation of copper accumulation in the liver tissue is the method of choice for diagnosis of Wilson’s disease. In patients with active disease or regenerative liver nodules, the copper in the liver may display normal values, while in those with cholestatic syndromes, the values may be high showing "false positive".
• Kayser-fleischer rings (seen during slit-lamp examinations) are not seen in 50% of those with WD and in asymptomatic siblings. However, these rings, which are typical of WD, are also seen in those with primary biliary cirrhosis.
• Neurologic evaluations - WD patients also show neurologic symptoms like those of Parkinson’s disease such as rigidity, dystonia or tremor. The patients should be thoroughly evaluated by a neurologist to confirm or rule out Wilson’s disease.
• Radiologic Imaging of the brain - Imaging studies such as the MRI can detect lesions and other abnormalities in the brain that are features of Wilson’s disease. These include the typical feature of Wilson’s disease described as the “face of the giant panda”.
• Genetic Testing - There are several mutations involved in bringing about Wilson’s disease therefore, genetic tests are not feasible. However, a study for the mutation in the gene ATP7B can be carried out once a provisional diagnosis of WD has been made.
• Liver function tests - These tests detect acute liver damage due to Wilson’s disease. It is important to detect liver damage due to Wilson’s disease, as the related death rate is phenomenally high. Simple and accurate methods include laboratory tests to evaluate the levels of alkaline phosphatase levels, bilirubin and serum amino transferases. These tests must not be considered alone but must be considered along with other signs and symptoms of Wilson’s disease.
• Family screening - When a patient has been identified with Wilson’s disease it is important to screen the family members as the likelihood of a sibling being homozygous for the disease is 25%. The chance of an offspring having the disease is 0.5%. Although the risks are low, genetic tests for close family of an affected person is justified considering the devastating course of the disease.
Treatment
Once Wilson’s disease is diagnosed, the treatment is life long. A number of drugs are available to treat Wilson’s disease.
They include:
• D-Penicillamine - This drug is used in those with WD to enhance the excretion of urinary copper. It is best taken one hour before meals, as food tends to interfere with the drug’s absorption. D-penicillamine interferes with pyridoxine action and therefore pyridoxine supplements must be administered.
Adequecy of treatment is monitored from the start of treatment by checking the 24-hr urinary copper excretion.
In patients with liver disease, the improvement in symptoms occurs typically in the first 2-6 months. In those patients with neurologic symptoms the improvement is much slower. Worsening of symptoms in the latter group has also been reported.
Side- effects of the drug include fever, skin eruptions, swelling of lymph nodes, or reduced blood counts. These can be seen in 30% of patients administered with the drug. Other side effects include kidney damage and a lupus-like syndrome. When the side effects appear, drug administration has to be stopped.
• Trientine - Trientine, a chelator, was introduced as an alternative to D-penicillamine and like the earlier drug, promotes urinary copper excretion. Trientine can be administered one hour before meal or three hours after meals. It may be used in patients developing side effects to D-penicillamine. The drug is effective in treating WD although side-effects, including neurologic worsening and reversible sideroblastic anemia, have been reported.
• Ammonium tetrathiomolybdate (TM) - This drug acts in a different way in that it interferes with the uptake of copper from the intestinal tract. As yet, clinical experiments with the drug are limited.
• Zinc - Like TM, zinc interferes with the uptake of copper from the digestive tract. It can give rise to side-effects. Besides being an immunosuppressant, zinc can act as a gastric irritant.
• Orthoptic Liver Transplantation (OLT) - OLT seems to be the only treatment option for those with acute liver disease or cirrhosis due to Wilson’s disease.
Prognosis
Wilson’s disease can be fatal if left untreated.
Prognosis of WD often depends on the severity of the liver and neurologic diseases and on the patients’ response to various treatments. Usually WD patients with liver disease do not respond well to treatment. On the other hand, those patients who present with neurologic symptoms fare much better than those that present with hepatic diseases.
Reference: Journal of hepatology 2012 VOL 56, 671-685
Source-Medindia








