Dalcetrapib does not improve the cardiovascular condition in patients with coronary artery disease.
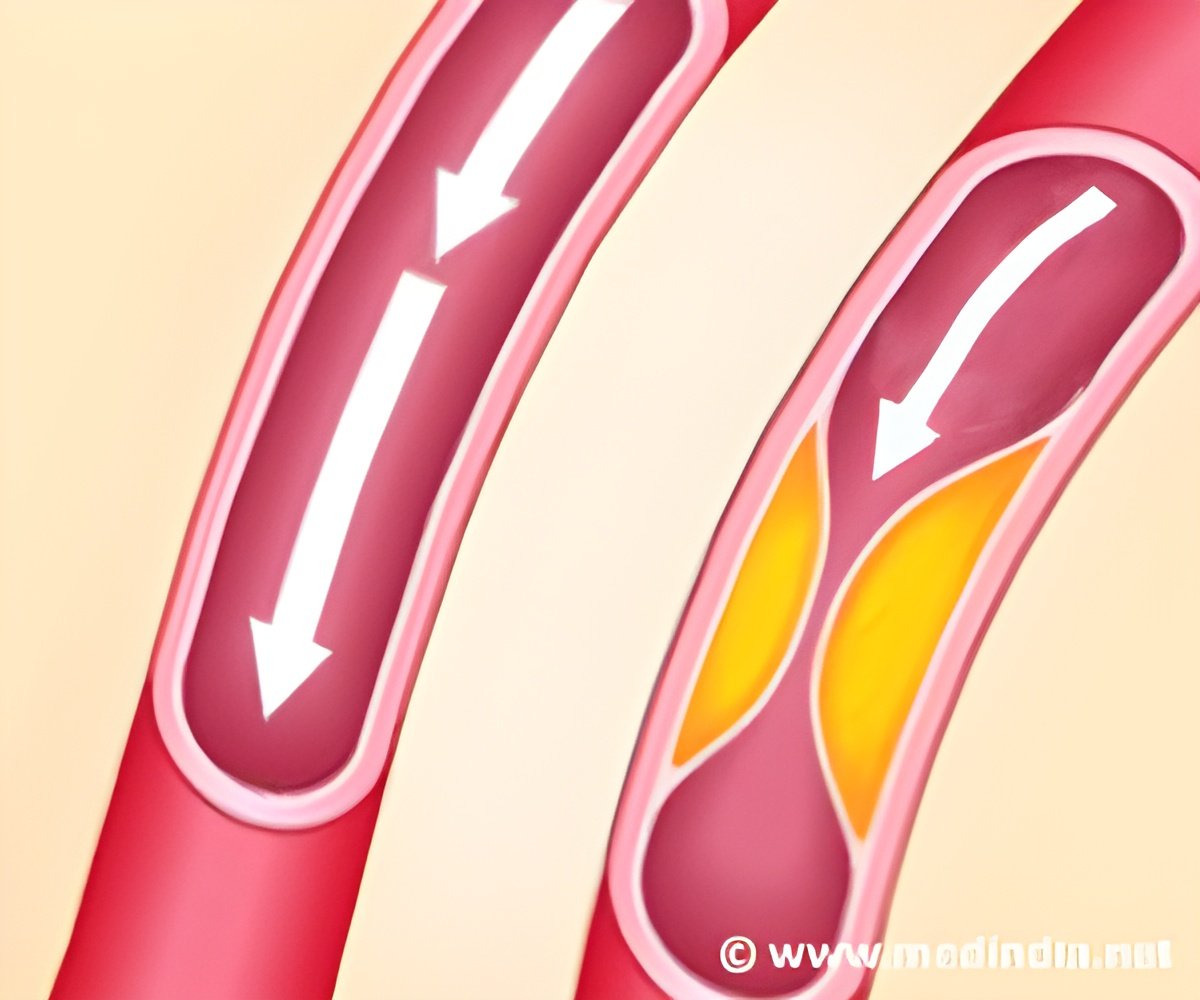
Taking the above into consideration, newer drugs are now being developed that could increase the levels of HDL, and thereby improve cardiovascular health. These drugs belong to a group that is referred to as the cholesteryl ester transfer protein (CETP) inhibitors. The first among these called torcetrapib was found to increase HDL cholesterol by more than 70% and decrease LDL cholesterol by 25%. Unfortunately, it was associated with deaths and morbidity due to a concomitant increase in the levels of the hormone aldosterone and blood pressure.
Another CETP inhibitor drug dalcetrapib has been found to increase HDL level by 30%, without similar side effects in a small study. Therefore, researchers conducted a bigger study to evaluate the effects of this drug in patients with a recent acute coronary syndrome (conditions affecting the blood supply to the heart). These included people who showed the presence of increase in markers of cardiac disease, symptoms of angina or heart attack, new changes in the ECG, or damage to the heart muscle as seen on imaging studies. In addition, patients with a recent heart attack who had undergone angioplasty were also included in the study.
The study enrolled 15,871 patients from 27 countries. The patients included in the study received either dalcetrapib 600 mg daily or a matching placebo. The study was terminated before the stipulated time at 31 months when the futility of continuing the trial was agreed upon.
Treatment with dalcetrapib increased the HDL cholesterol levels from 31 to 40% with minimal effect on LDL cholesterol level. However, this increase in HDL levels was not associated with a decrease in deaths or incidence of coronary heart disease or unanticipated coronary revascularization procedures (like angioplasty). In fact, the group that received dalcetrapib showed a significant increase in C-reactive protein level, which reflects the proinflammatory effect of the drug and ability to cause increased cardiovascular events.
The mean systolic blood pressure was significantly higher in the group that received dalcetrapib as compared to the group that received placebo. Diarrhea was also more common in the dalcetrapib group, thus contributing to its discontinuation. In addition, patients also complained of insomnia.
• It is possible that HDL levels are not protective in patients who were receiving other treatments like statins, antiplatelet therapy, beta-blockers, ACE inhibitors or ARBs, and coronary revascularization procedures.
• It is also not known if dalcetrapib affected the function of HDL.
• The favorable effects of dalcetrapib may also have been offset by the side effects of treatment like a rise in systolic blood pressure and an increase in C-reactive protein level.
Thus, though dalcetrapib increased HDL levels, it did not result in a significant decrease in cardiovascular events in patients with coronary artery disease. The utility of such drugs thus remains questionable.
Reference:
1. Effects of Dalcetrapib in Patients with a Recent Acute Coronary Syndrome; Gregory Schwartz et al; N Engl J Med 2012; 367:2089-2099
Source-Medindia