Monogenic hereditary disorders are largely responsible for child mortality and morbidity. However, intrauterine genetic editing could correct the genetic defect and thereby cure the disease in the fetus.
- Children born with β-thalassemia require a lifetime of blood transfusions, iron chelation therapies and medications to survive as there is no permanent cure
- In this study, in utero genetic editing of the β-globin gene was investigated in a mouse model of human β-thalassemia
- This intervention corrected the genetic defect and can be a potential cure for such monogenic disorders in fetuses
Can In Vivo Gene Editing Cure Blood Disorders in Fetus ?
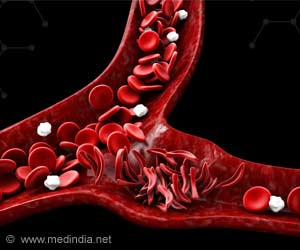
Thalassemia can be detected in early pregnancy using invasive techniques like CVS (chorionic villi sampling). Recent advances in NIPT (non-invasive prenatal testing) make it easier to diagnose a fetus with β-thalassemia major. Advances in gene therapeutics have made it possible to cure thalassemia using a viral vector to replace mutated copies of the β-globin gene with healthy copies. However, there are challenges with the use of viral vectors as a mode of healthy gene delivery.The team of researchers in this study demonstrated in utero genetic editing of the β-globin gene in a mouse model of human β-thalassemia. The team used intravenous injections of polymeric, biodegradable nanoparticles (NPs) carrying triplex-forming peptide nucleic acids (PNAs) and single-stranded donor DNAs to correct the defective gene.
The research group had previously demonstrated genetic correction of β-thalassemia and cystic fibrosis with PNA/DNA NPs. In this study, the group showed how endogenous genome editing can be carried out effectively and safely in vivo without any detectable off-target mutations.
Is In Utero Gene Editing Safe ?
In this study, the main objective was to determine the safety, efficacy and feasibility of in utero gene editing using PNA/DNA-containing NPs. The study found that NPs can be delivered to multiple fetal mouse tissues via intravenous infusions with significant accumulation in the fetal liver (which is the site of hematopoiesis).The research team used NPs loaded with next-generation, chemically modified γPNAs and DNAs to correct the disease-causing mutation in utero. After in utero correction, the team observed post-natal improvement in fetal mice with the elevation of hemoglobin levels, improved red cell morphology, decreased reticulocyte counts and reduction in extramedullary hematopoiesis.
The study implies a survival advantage for in utero treated animals versus the untreated animals in the control group.
The research has provided the foundation for site-specific gene editing in utero using γPNA/DNA nanoparticles. Further studies are required to validate safety and efficacy in other disease models including animals like non-human primates. The research has tremendous potential clinical translational applications for human genetic disorders.
- Ricciardi, Adele S., Raman Bahal, James S. Farrelly, Elias Quijano, Anthony H. Bianchi, Valerie L. Luks, Rachael Putman et al. "In utero nanoparticle delivery for site-specific genome editing." Nature communications 9, no. 1 (2018): 2481. Accessed on July 6, 2018 from (https://www.nature.com/articles/s41467-018-04894-2)
Source-Medindia