A new study has shown that liver transplant recipients with less understanding of the treatment may be more likely to have trouble following the prescribed regimen.
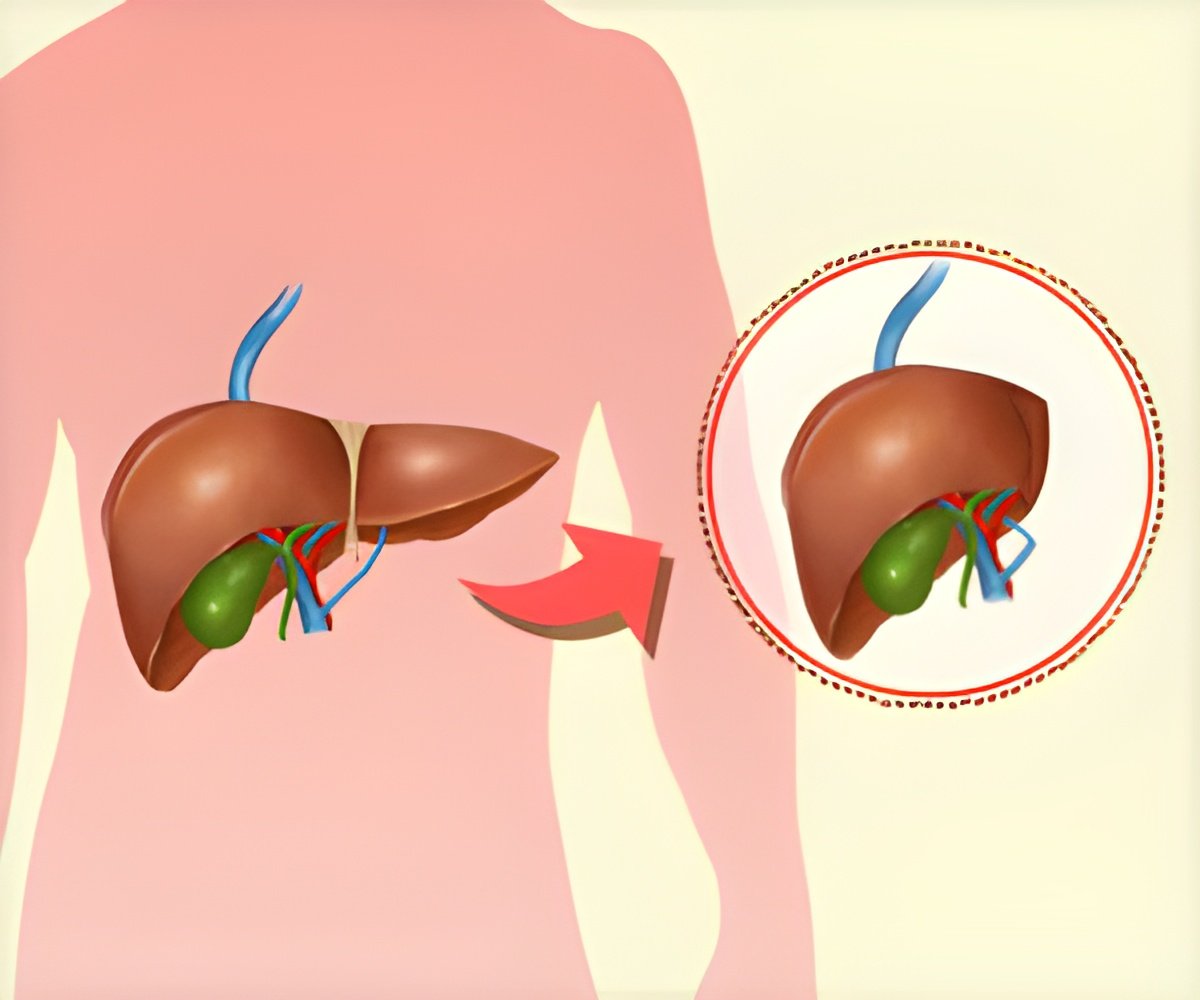
The study published in the journal liver transplantion included 105 post-liver transplantation middle-aged males, who were each prescribed 11 drugs on an average. Around 15% of the patients had limited literacy.
The researchers found that limited literacy and taking more medications were associated with non-adherence to the treatment. The self-reported non-adherence was recorded as 14%; when the blood levels of tacrolimus, one of the medication used post-transplantation was measured, this number jumped to 32%.
Dr. Marina Serper from the Hospital of the University of Pennsylvania in Philadelphia, says that, “It is important to understand how crucial self-care behaviors, such as following treatment plans, could lead to re-hospitalization, graft rejection, and infection if post-transplant regimens are not followed,” added Dr. Serper.
Dr. Serper concludes, “Higher scores for treatment knowledge and demonstrated regimen use were independently associated with reduced post liver transplant re-hospitalization.
Also, we could see an enhancement in long-term health of liver recipients involving existing transplant center resources in cost-effective interventions that help patients properly supervise their drug regimens.”
The interventions that are effective in improving liver recipients’ adherence to the medical regimen include:
- Counseling on antirejection medication in the hospital.
- Educational intervention for paediatric patients.
- Increasing the frequency of clinical visits for nonadherent patients.
- Providing the liver recipients with a dedicated psychoeducational service.
After a liver transplant what are the signs of organ rejection that transplant patients need to watch out for?
The vast majority of rejection episodes are asymptomatic and detected on regular screening labs. In advanced cases, symptoms of liver rejection include:- Itching
- Jaundice - yellow skin and yellowing of the whites of the eyes
- A high temperature of 38ºC (100.4ºF) or above
- Vomiting
- Diarrhoea
- Pale stools
- Dark urine
There are three major immunosuppressive drugs commonly used in transplant, each with its own set of potential side effects:
- Tacrolimus - Tacrolimus can cause kidney damage, high blood pressure, diabetes and neurologic disturbances.
- Mycophenolate - Mycophenolate can cause stomach upset, diarrhea and bone marrow suppression (low white blood cell count).
- Prednisone - Prednisone can cause diabetes, weight gain and poor wound healing.
All of the immunosuppressive drugs together increase the risk of infection and cancer. It is important to have regular checkups with the transplant team to assess the new liver’s function, to look for any drug side effects and to examine for signs of infection or cancer.
Brief overviews of drug interactions in liver transplant patients
Drug interactions with immunosuppressive medications can occur with certain antimicrobial drugs particularly antifungal agents - certain seizure medications and certain antiviral medicines.It is important that the Transplant Pharmacist regularly review the patient’s medication list to look for potential drug interactions or drug dosage adjustments that might be necessary.