Excess LDL cholesterol causes atherosclerotic cardiovascular disease but reducing its levels prove to benefit people with this disease.
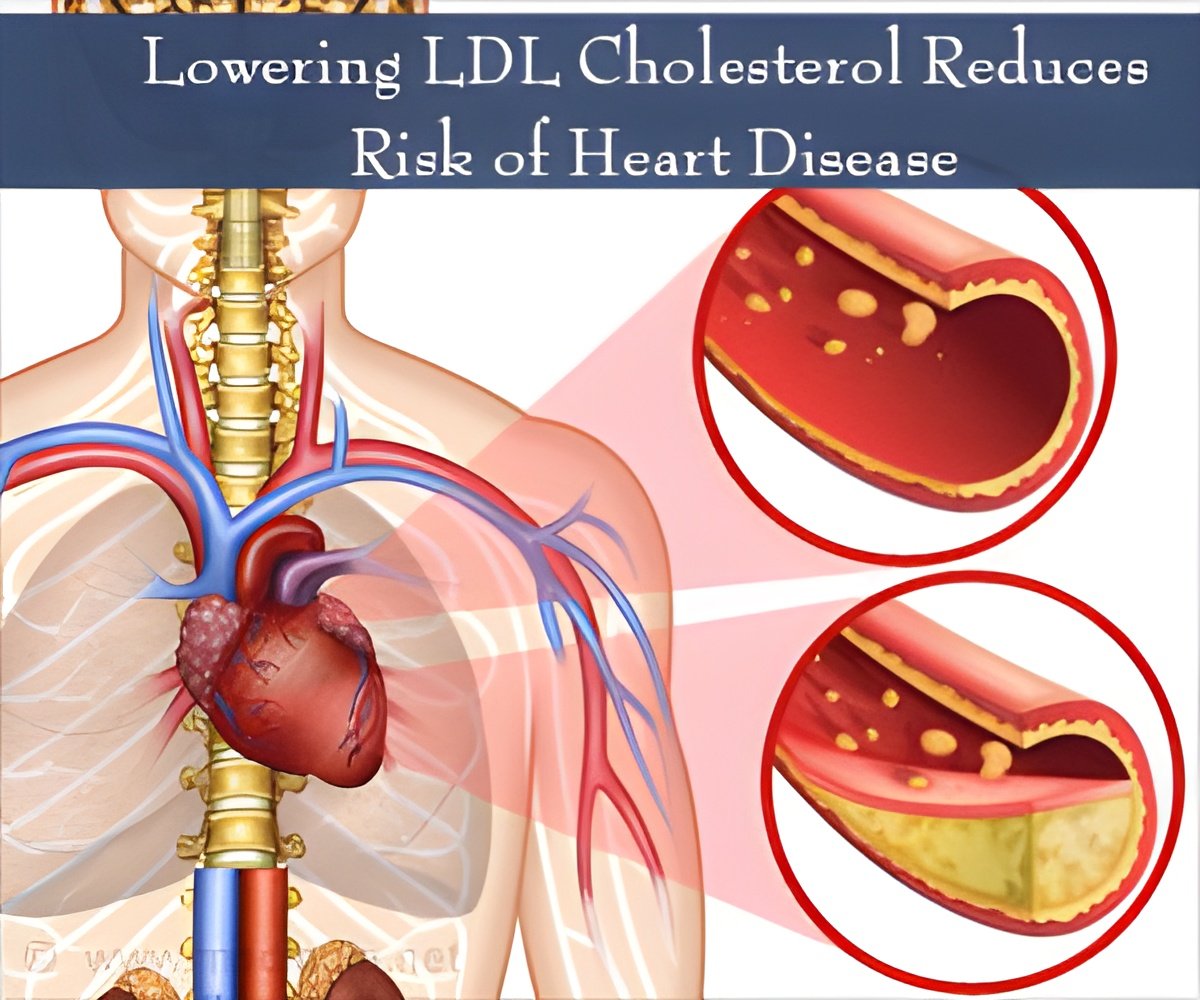
In an editorial published in The New England Journal of Medicine on 18 June, 2015, Jarcho and Keaney analyze the reports of the IMPROVE-IT study in favour of the LDL hypothesis. The IMPROVE-IT trial (Improved Reduction of Outcomes: Vytorin Efficacy International Trial) aims at comparing ezetimibe/simvastatin combination therapy with simvastatin alone in high-risk patients with severe coronary syndromes. The results of the study confirmed that combining a non-statin lipid-lowering drug with a statin can have additional benefits in lowering LDL cholesterol levels thereby reducing adverse cardiovascular events. The addition of a non-statin agent (ezetimibe) to statin therapy reduced the absorption of cholesterol from the gastrointestinal tract and lowered LDL cholesterol by 24%.
In the IMPROVE-IT trial, 18, 144 patients with acute coronary syndrome were randomly assigned to either simvastatin (40 mg) plus ezetimibe (10 mg) or to simvastatin (40 mg) plus placebo. After 1 year, the mean LDL cholesterol level was 53.2 mg per decilitre in the simvastatin-plus-ezetimibe group and 69.9 mg per decilitre in the simvastatin monotherapy group. The primary endpoint in the trial was a range of adverse cardiovascular events like myocardial infarction, unstable angina, cardiovascular death or nonfatal strokes. After 7 years, the rate of the primary endpoint was lower by 2.0 percentage points in the simvastatin-plus-ezetimibe group.
The results of IMPROVE-IT provide hope to patients who do not respond sufficiently well to statin therapies. While the 2013 cholesterol treatment guidelines of the American College of Cardiology and the American Heart Association do not recommend specific agents to reduce LDL levels, it acknowledges the need to add a non-statin agent when patients do not respond to statin therapy alone.
The IMPROVE-IT study also suggests that reduction in LDL cholesterol is beneficial, regardless of the agent used. The recent development of PCSK9 inhibitors is highlighted. These agents enable LDL clearance from blood circulation and reduce LDL cholesterol by almost 60%. Clinical trials with these agents are in process.
IMPROVE-IT does not specifically prove unique benefits of ezetimibe, rather it suggests that reduction in LDL cholesterol by any mechanism is useful to prevent adverse cardiovascular events.
References
1. Jarcho, A. John & Keaney, F. John. (2015). “Proof That Lower Is Better — LDL Cholesterol and IMPROVE-IT”. New England Journal of Medicine 18 June 2015: 372:2448-2450. DOI: 10.1056/NEJMe1507041. Retrieved on 21 September 2015 from http://www.nejm.org/doi/full/10.1056/NEJMe15070412. http://www.escardio.org/Congresses-&-Events/Upcoming-congresses/ESC-Congress/Congress-news/low-density-lipoprotein-cholesterol
4. http://www.nejm.org/doi/full/10.1056/NEJMoa1410489#t=articleTop
5. http://www.timi.org/index.php?page=improve-it-timi-40
6. https://www.bhf.org.uk/heart-health/risk-factors/high-cholesterol
7. http://www.fda.gov/ForConsumers/ByAudience/ForWomen/ucm118595.htm
Source-Medindia