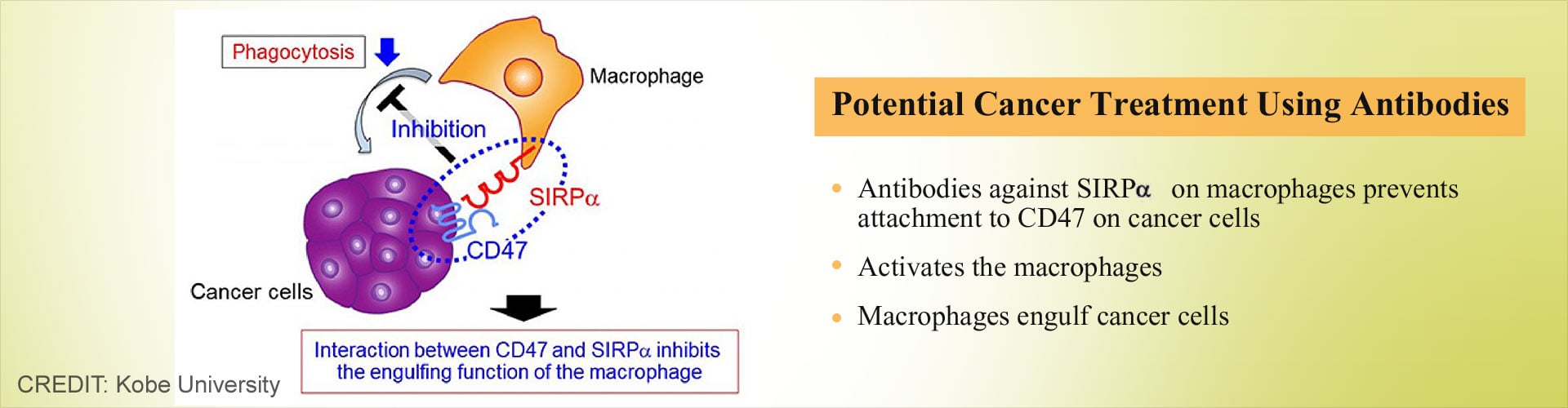
Scientists discover that antibodies against protein on macrophages activates these cells to engulf cancer cells, providing a potential cancer treatment.
- A research team from Kobe University has found that disruption of SIRPα- CD47 could activate macrophages.
- Antibodies for SIRPα activated macrophages engulfed tumor cells when the drug rituximab was administered.
- This provides a potentially new method of treatment for cancer.
New cells in the body are formed when the body requires them and once a cell gets in contact with another cell, it stops growing. However, in cancer, the cells continue to grow and develop, even when there is no requirement, with a loss of contact inhibition. In cancer, the new cells start forming but the old cells do not die; the additional cells grow into a mass of cells known as tumor. There are over 100 different types of cancer cells and they are named based on the site of origin.
Since the cancer cells are the body’s own cells, they are not recognized by the body’s immune system as foreign and fail to mount an effective immune response. The current study focuses on activating macrophages, which are a type of white blood cells capable of destroying cancer cells.
SIRPα on Macrophages
Earlier studies by the same research team found that the SIRPα expressed on the surface of the macrophages are suppressed by the CD47 expressed on the cancer cells, thus resulting in poor fight against the cancer cells. Studies on immunodeficient mice were carried out by injecting Raji cells that were from human B cell lymphoma. The study found that
- An antibody to SIRPα that binds to SIRPα and prevents interaction with CD47 aided rituximab in suppressing tumor growth..
- The antibodies against SIRPα could be highly effective against tumors by improving phagocytosis of macrophages using cancer drugs like rituximab..
- Human and mice renal carcinoma and melanoma cells expressed high levels of SIRPα
- Mice that were injected with mouse melanoma or renal cell carcinoma (RENCA) cells showed suppressed tumor growth when antibodies to SIRPα were administered. .
- Mice in which macrophages were removed showed poor suppression of antibodies to SIRPα.
The PD1 protein or the programmed cell death protein is expressed on the surface of β-cells and plays an important role in their differentiation. The protein is also found to be important in T-cell function and is also associated with the prevention of autoimmune diseases.
The findings of the study suggest that
- Antibodies against SIRPα act as an immune checkpoint for macrophages in the innate immune system.
- This has potential use as new cancer treatment with antibodies to SIRPα developed as a drug therapy for cancer.
Mice that expressed SIRPα variants with the capacity to attach to human CD47 were studied and the experiments showed that macrophage induced phagocytosis and removal of acute myeloid leukemia stem cells were due to disruption of SIRPα signaling.
These findings have shown that the development of drug therapy that involves disruption of SIRPα signaling, activating macrophage-mediated elimination of tumor cells would be effective in tumor suppression.
References:
- Cancer - (https://medlineplus.gov/cancer.html)
- What is the Science of PD-1 and Immunotherapy? - (http://blog.dana-farber.org/insight/2015/05/the-science-of-pd-1-and-immunotherapy/)
- PDCD1 programmed cell death 1 - (https://www.ncbi.nlm.nih.gov/gene/5133)
- Disruption of SIRPα signaling in macrophages eliminates human acute myeloid leukemia stem cells in xenografts. - (https://www.ncbi.nlm.nih.gov/pubmed/22945919)
Source-Medindia