Avoiding rampant use of antibiotic combinations and refraining from early therapy with ‘last resort’ drugs will reduce emergence of drug resistant strains.
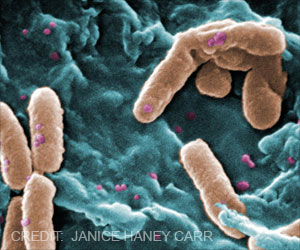
- Emergence of drug-resistant carbapenemase-producing Enterobacteriaceae (CPE) infections is a major threat and can increase mortality rates.
- Avoiding unnecessary use of antibiotic combinations in patients with bloodstream infections can reduce the incidence of adverse effects and emergence of drug resistance.
- Desisting from the use of powerful ‘last measure’ antibiotics such as carbapenems to initiate early therapy for low-risk infections is critical to reduce the development of drug resistant bacteria.
Aims of The Two Studies
- The first study aimed to determine the effects of treating with a combination of antibiotics in patients with bloodstream infections caused by carbapenemase-producing Enterobacteriaceae (CPE).
- The second study wished to determine the effects of starting therapy with antibiotics other than carbapenems in bloodstream infections with extended-spectrum beta-lactamase producing Enterobacteriaceae (ESBL-E), which are resistant
- To many antimicrobial drugs including cephalosporins.
Methods And Findings of the Two Studies
Study 1 In the first presentation, Professor Jesús Rodríguez-Baño, Head of the infectious diseases division at the University Hospital Virgen Macarena (Seville, Spain) and President-elect of the European Society of Clinical Microbiology and Infectious Diseases (ESCMID), presented findings from 37 hospitals in 11 countries on 437 patients with bloodstream infections caused by CPE -- a group of bacteria that are resistant to carbapenems. These can kill approximately half of the patients who develop bloodstream infections.Fifty-one percent of the patients were low risk.
- During the study, 343 patients received antimicrobial treatment active against the organism responsible for the infection -- either a single antimicrobial drug or a combination.
- This treatment reduced the mortality risk of the entire group by more than 50%.
- However, combination therapy showed a reduced risk of death (a decrease of 44%) only in the high-risk patients, and not in the low-risk patients.
This helps to avoid the problems due to combination therapy, such as a higher risk of toxicity, the development of resistance by the infectious agents to more antimicrobials, and the bigger cost.
The study therefore suggests that combination therapy is reserved only for high-risk patients with CPE bloodstream infections.
STUDY 2
Dr Palacios Baena and her colleagues studied 855 patients with bloodstream infections caused by ESBL-E treated between 2004 and 2012 in the INCREMENT study and who received their first dose within 24 hours before antibiotic sensitivity results became available.
- Patients were again categorized as low risk and high risk categories based on the probability of their dying within 30 days.
- The patients who started
antimicrobial therapies before the sensitivity of the organism was known
were classified into three groups:
- Patients who were given "choice therapy (CT)" - Carbapenems or another broad spectrum antimicrobial therapy called beta-lactamase/beta-lactamase inhibitors; these patients were used as the reference group to compare with the other two groups.
- Patients who were given "alternative therapy (AT)"- Other antimicrobial agents, either alone or in combination, which were known to be effective against ESBL-E in the laboratory.
- Patients who were given "inactive therapy (IT)" - Antimicrobial therapy that proved to be inactive against the infection.
- A total of 144 patients (17%) died.
- The death rates for CT patients was 17%, for AT patients it was 19%, and for IT patients, 15.5% showing no statistically significant difference in the death rates of the 3 groups.
- The risk of death in high-risk patients rose by a third for each point increase on the INCREMENT-ESBL score. The patients treated with inactive therapy had a nearly three-fold increased risk of death.
With recent advances in diagnostic techniques, antibiotic sensitivity results are available within 24 hours and even if initial treatment was inactive, doctors can switch to the targeted active drug soon enough.
Though further studies may be needed to validate these findings, carbapenem resistance can be reduced by avoiding its use in select patients.
References:
- Belén Gutiérrez-Gutiérrez, Elena Salamanca, Marina de Cueto, Po-Ren Hsueh, Pierluigi Viale, José Ramón Paño-Pardo, Mario Venditti, Mario Tumbarello, George Daikos, Rafael Cantón, Yohei Doi, Felipe Francisco Tuon, Ilias Karaiskos, Elena Pérez-Nadales, Mitchell J Schwaber, Özlem Kurt Azap, Maria Souli, Emmanuel Roilides, Spyros Pournaras, Murat Akova, Federico Pérez, Joaquín Bermejo, Antonio Oliver, Manel Almela, Warren Lowman, Benito Almirante, Robert A Bonomo, Yehuda Carmeli, David L Paterson, Alvaro Pascual, Jesús Rodríguez-Baño, M D del Toro, J Gálvez, M Falcone, A Russo, H Giamarellou, E M Trecarichi, A R Losito, E García-Vázquez, A Hernández, J Gómez, G Bou, E Iosifidis, N Prim, F Navarro, B Mirelis, A Skiada, J Origüen, R San Juan, M Fernández-Ruiz, N Larrosa, M Puig-Asensio, J M Cisneros, J Molina, V González, V Rucci, E Ruiz de Gopegui, C I Marinescu, L Martínez-Martínez, M C Fariñas, M E Cano, M Gozalo, M Mora-Rillo, C Navarro-San Francisco, C Peña, S Gómez-Zorrilla, F Tubau, A Tsakris, O Zarkotou, A Antoniadou, G Poulakou, J Pitout, D Virmani, J Torre-Cisneros, J Guzmán-Puche, Ö Helvaci, A O Sahin, V Pintado, P Ruiz, M Bartoletti, M Giannella, E Tacconelli, F Riemenschneider, E Calbo, C Badia, M Xercavins, O Gasch, D Fontanals, E Jové. Effect of appropriate combination therapy on mortality of patients with bloodstream infections due to carbapenemase-producing Enterobacteriaceae (INCREMENT): a retrospective cohort study. The Lancet Infectious Diseases, (2017); DOI: 10.1016/S1473-3099(17)30228-1
Source-Medindia