Early stem cell therapy in stroke patients aids better recovery by reducing infections and unwanted and harmful inflammation.

- Stroke is a leading cause of death and chronic disability in elderly patients
- Recovery in stroke patients hampered by serious infections and tissue damage due to an exaggerated immune response
- Early stem cell therapy aids better recovery in stroke patients by modulating the immune response
- Stem cell therapy is safe and well-tolerated in stroke patients
Why Give Stem Cells in Stroke Patients
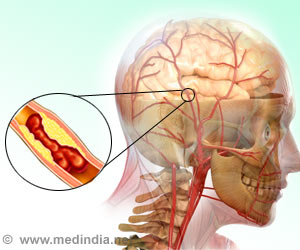
Recovery in stroke patients can be affected by increased risk of infections and tissue damage, due to unnecessary destructive inflammation. Stem cell therapy, especially if given early, can modulate the immune response and promote better recovery in the long-term.Details of the Study
- The study was conducted between October 2011 and December 2015 in 33 centers across the United Kingdom and the US. Patients included 129 adults with moderately severe stroke.
- A dose of 400 million cells was administered initially to a handful of patients to establish safety. Following this, the dose was increased to 1,200 million cells for most of the patients.
- While half the patients received the stem cells, the remaining received placebo.
- Both groups of patients had received conventional treatments including tissue plasminogen activator (tPA) to dissolve the clot, or an endovascular operation to remove it.
- The timing of the therapy ranged between 24-48 hours, though earlier animal studies indicate that 24-36 hours was the optimal time for the treatment. This was due to some centers needing more time to thaw and prepare the stem cells.
Results of the Study
The patients were initially followed up at three months but 80 percent of the volunteers were followed up at one year.Results indicated that in the long-term, patients who had received stem cell therapy continued to recover with decreased incidence of infections and lesser disability compared to the placebo group.
"There is solid evidence from our basic science work and now some indicators from this phase 2 patient trial that giving these stem cells can safely help dial back the body's immune response to stroke injury that can ultimately further damage the brain and body," said Dr. David C. Hess, stroke specialist and chairman of the Department of Neurology at the Medical College of Georgia at Augusta University.
Early animal studies, conducted by former MCG neuroscientist Dr. Cesario V. Borlongan, pediatric neurologist and professor emeritus Dr. James Carroll and Hess, showed that the stem cells would be most beneficial if administered within two days of an ischemic stroke and could reduce death of cells adjacent to the stroke's core, that were also injured.
How the Stem Cells Help Recovery
The stem cells used in the trial were multipotent stem cells, dubbed Multistem. Interestingly, the dose administered was the largest ever in a human cell therapy trial. These cells are safe and literally ‘off the shelf’, requiring no tissue typing. A single donor can provide several thousand doses to patients. They were well-tolerated, and side effects in a few patients included fever, chills, bad breath, nausea and vomiting.However, in stroke patients, the spleen,an important organ of the immune system shrinks in size. As a result it dumps large quantities of activated immune cells into the bloodstream, which could travel to the brain and cause destructive inflammation there.
"Some inflammation is good, but in a big stroke, it almost always overshoots," Hess said of
this second neuroinflammatory response. "We think this secondary neuroinflammatory process is preventing the natural healing tendencies of the body."
Patients who received stem cell therapy were found to have lower blood levels of inflammatory mediators called cytokines, as well as other drivers of the immune reaction, including circulating lymphocytes and a subset of lymphocytes called regulatory T cells.
Future Research Plans
Following this current phase 2 clinical trial, the research team plans to conduct further studies in the UK, US, Europe and Japan as well where there is a significant aging population before seeking FDA approval.- They hope to limit the timing of the therapy to 18-36 hours with centers now equipped with faster means of stem cell preparation and thawing.
- They plan to measure the spleen size of the patients before and after therapy
- They also plan to correlate increased blood levels of cytokines with tissue levels.
- During the phase 2 study itself, the age limit for giving cell therapy was increased from 79 to 83.
- Also, the patients included in the stem cell trial was expanded to include patients who had received both tPA and endovascular clot retrieval rather than one of the two, since many centers performed clot retrieval.
References:
- David C Hess, Lawrence R Wechsler, Wayne M Clark, Sean I Savitz, Gary A Ford, David Chiu, Dileep R Yavagal, Ken Uchino, David S Liebeskind, Alexander P Auchus, Souvik Sen, Cathy A Sila, Jeffrey D Vest, Robert W Mays. Safety and efficacy of multipotent adult progenitor cells in acute ischaemic stroke (MASTERS): a randomised, double-blind, placebo-controlled, phase 2 trial. The Lancet Neurology, (2017); DOI: 10.1016/S1474-4422(17)30046-7
Source-Medindia