Researchers have developed a blood test that sequences tiny bits of circulating tumor DNA to diagnose and manage diffuse large B-cell lymphoma.
Highlights
- Patients with diffuse large B-cell lymphoma require repeated lymph node biopsies to diagnose and follow up the patient for recurrence following treatment
- Researchers offer a simple blood test that sequences tiny bits of circulating tumor DNA and helps to diagnose the subtype as well as to follow up the cancer
- The findings of the research could simplify the management and increase efficacy of treatment in these patients
Diagnosis of diffuse large B-cell lymphoma requires a lymph node biopsy. Treatment is with chemotherapy, radiation and/ or stem cell transplantation. The response to treatment varies with different subtypes of the cancer. While some forms are curable, others are extremely difficult to treat.
Researchers sequenced tiny bits of DNA from the blood of 92 patients with diffuse large B-cell lymphoma. They used a technique called CAPP-Seq to identify several mutations in the tumor gene and have found that they provide the following information:
- The cancer subtype can be determined through the sequencing test. Since the treatment and prognosis depends on the cancer subtype, this information is extremely important. For example, patients with germinal center subtype have a better prognosis as compared to those with activated B-cell-like tumors. Since the subtypes respond differently to treatment, the treatment can be individualized based on this information.
- Mutations that may be associated with drug resistance can be detected. This helps in deciding the choice of chemotherapy medications which will work best for the patient. The researchers detected mutations which may determine resistance to the anticancer medication ibrutinib.
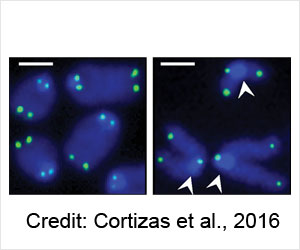
- The level of circulating tumor DNA before treatment is an indicator of the prognosis of the cancer. Patients with lower initial circulating tumor DNA levels have better chances of progression-free survival, while those with higher levels are likely to have poorer outcomes.
- Repeated testing helps to detect any remaining cancer following treatment and turned out to be better than radiological tests for the same. It also detects changes in the sequences over time which may indicate worsening of the cancer into a more aggressive form. This information could be used to change the treatment into a more intensive type to deal with the cancer. In fact, repeated sequencing enabled researchers to detect a relapse in the cancer at an average of six months before the appearance of any symptoms.
Reference:
- Scherer F et al. Distinct biological subtypes and patterns of genome evolution in lymphoma revealed by circulating tumor DNA. Science Translational Medicine 09 Nov 2016: Vol. 8, Issue 364, pp. 364ra155 DOI: 10.1126/scitranslmed.aai8545