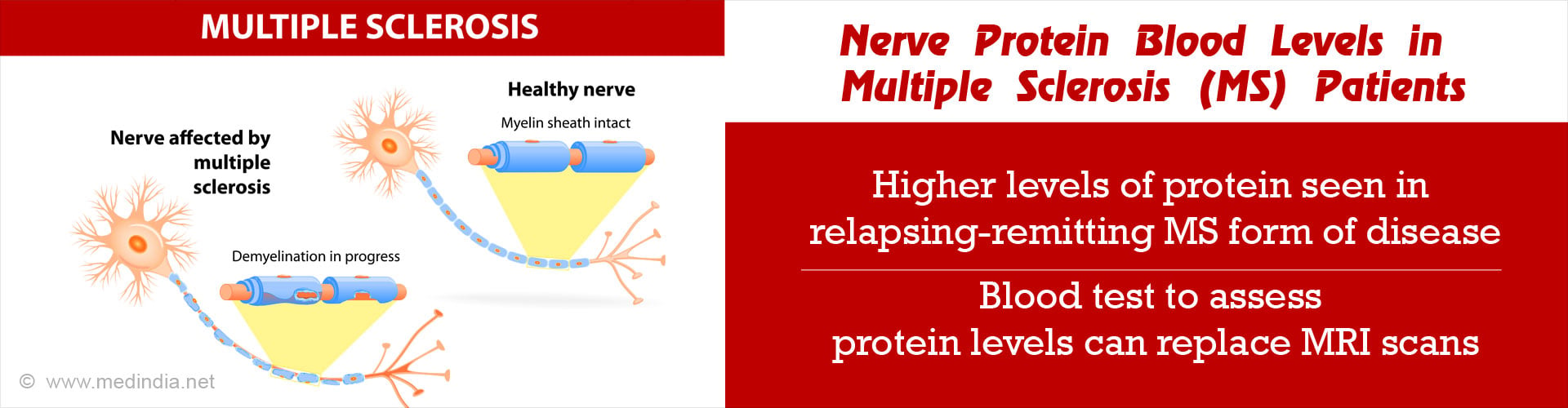
A blood test that detects the presence of a nerve protein in the blood is indicative of multiple sclerosis flare-ups.
- New disease activities in multiple sclerosis patients detected through MRI now correlate with the presence of a nerve protein in the blood.
- Relapsing-remitting multiple sclerosis is characterized by surges of neurological symptoms followed by periods of remission.
- The nerve protein is likely to make its mark as a new biomarker and the blood test as a cost-effective alternative to MRI.
"Since MS varies so much from person to person and is so unpredictable in how the disease will progress and how people will respond to treatment, identifying a biomarker like this that can help us make predictions would be very helpful," said study author Kristin N. Varhaug, MD, of the University of Bergen in Bergen, Norway. "These blood tests could provide a low-cost alternative to MRI for monitoring disease activity."
Study conducted on patients with relapsing-remitting MS
Relapsing-remitting MS (RRMS) is a form of MS where patients experience flare-ups of their neurological symptoms followed by periods of no disease progression or remission.Study design
Eighty five patients with RRMS were monitored for an average period of two years.Treatment procedure: No disease-modifying treatment was given in the first six months. Interferon-beta 1a (which is known to reduce the number of flare-ups and the accumulation of brain lesions in MS), was given for the next eighteen months.
Magnetic resonance imaging (MRI): MRI scans were performed every month for the first nine months, after which, two scans were done, one at year one and the other at year two. The frequent MRI scans are a limitation of the study.
Blood tests: Blood samples were taken at the beginning of the study, at three months, six months, year one and year two.
Results of the study
The neurofilament light chain (NfL) levels were monitored during the two years and their blood levels were found to be higher (and present for a three-month time period) when the MRI detected new disease activity (characterized by T1 and T2 lesions in the brain that are known to occur due to MS).NfL blood levels were lower in patients when interferon beta 1a treatment was taken to reduce flare-ups.
Statistical results include:
- Level of NfL detected was 37.3 picograms per milliliter (pg/ml) when T1 lesions were present compared with 28 pg/ml for people without new T1 lesions.
- Level of NfL detected was 37.3 picograms per milliliter (pg/ml) when T2 lesions were present compared with 27.7 pg/ml for people without new T2 lesions.
- An increase of 10 pg/ml in a person was associated with a 48-percent increased risk of developing a new T1 lesion and 62-percent increased risk of developing a new T2 lesion.
Conclusion
The findings suggest that measuring the levels of NfL in the blood may be an effective way to monitor disease activity and to ascertain the effectiveness of treatment. Future studies may need to be done with extended follow-up times.Multiple sclerosis (MS)
Multiple sclerosis (MS) is a brain disorder in which the protective layer that covers the brain and spinal cord known as the myelin sheath is damaged. This leads to improper signalling of nerve messages in some parts of the brain. It mostly affects people in the age group between 20 and 50 and is more common in women. It is considered to be an immune-mediated process because the exact antigen or target that makes the immune system direct its action against the central nervous system (CNS is unknown.MS is known to surface in genetically predisposed people when there are exposed to certain environmental triggers. The patients experience one of four disease courses among which the relapsing-remitting MS (RRMS) is the most common course (85% of people with MS are initially diagnosed with RRMS).
In RRMS, there are clear defined attacks of new or increasing neurologic symptoms that are called relapses or exacerbations. These relapses are followed by partial or complete recovery periods or remissions. While in remission periods, symptoms may disappear, continue or become permanent but there is no apparent disease progression that takes place.
References:
- Kristin N. Varhaug, Christian Barro, Kjetil Bjørnevik, Kjell-Morten Myhr, Øivind Torkildsen, Stig Wergeland, Laurence A. Bindoff, Jens Kuhle, Christian Vedeler. Neurofilament light chain predicts disease activity in relapsing-remitting MS. Neurology - Neuroimmunology Neuroinflammation, 2017; 5 (1): e422 DOI: 10.1212/NXI.0000000000000422
- Multiple Sclerosis News & Research - (https://www.nationalmssociety.org/)