Scientists discover why lab generated induced pluripotent stem cells (iPSCs) derived from patient’s own adult cells such as skin cells get rejected by the immune cells when the stem cells are transplanted back into the same patient.
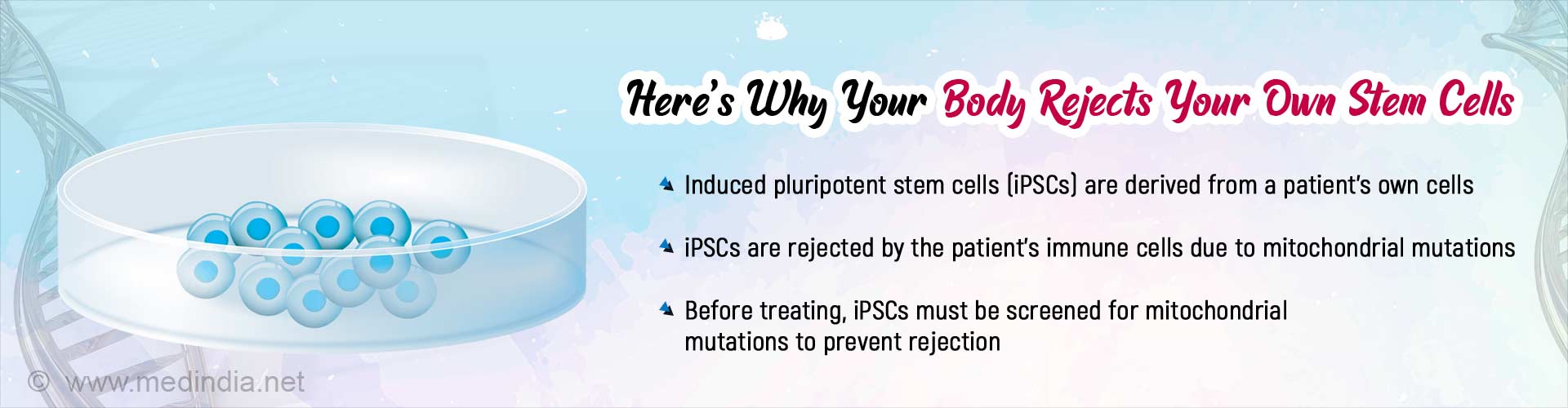
Highlights:
- Scientists discover why lab generated induced pluripotent stem cells (iPSCs) derived from patient’s own adult cells get rejected by the immune cells when the stem cells are transplanted into the same patient
- Since the same person would act as both the donor and the recipient of his cells, the iPSCs were believed to contain proteins or antigens that are identical and therefore would not be recognized and rejected by the person’s immune system
- During the conversion of adult skin cells to iPSCs, there is a mutation of DNA found in cytoplasmic structures called mitochondria. These mitochondrial mutations induce an immune response that makes humans and mice reject iPSC-derived cell transplants
The findings of the study appear in the journal Nature Biotechnology.
Role of Mitochondrial DNA in Cellular Activity
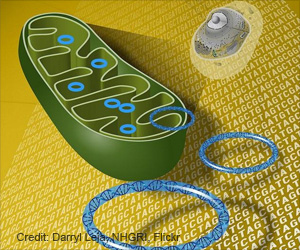
- Typically, mitochondria are cytoplasmic structures within the cell, where energy for almost all the biological processes in the body is produced, giving them the name “powerhouses of the cell”
- However, similar to DNA found within the nucleus (nuclear DNA), mitochondria also have another special function because they contain their own DNA and mitochondrial genes that encode for certain critical cellular proteins
- For example, in cells that are metabolically active, such as heart muscle cells, nearly 1/3rd of the cellular protein is encoded by mitochondrial genes. This means that a tiny mitochondrial gene mutation can have drastic consequences in these cells
- In the same manner, a small mutation in the mitochondrial DNA of a stem cell can cause a patient’s stem cell to be recognized as “foreign” and attacked by the patient’s own immune system
Proving that Mitochondrial Mutations Trigger Immune Rejection of Stem Cell Transplant
- The study team created hybrid stem cells with nuclear DNA from one mouse strain and mitochondrial DNA from a different mouse strain
- These hybrid stem cells were introduced into mice with similar nuclear DNA, but whose mitochondrial DNA was only slightly different
- A few days after transplant, the team obtained and harvested immune cells from the mice and exposed the immune cells to different fragments of the protein encoded by mitochondrial DNA
- It was found that the immune cells rejected the mitochondrial proteins they recognized as foreign
Replicating the Same Experiment in Humans
For obvious reasons, the above experiments can't be done in human subjects. However, the team adapted the experiment by enlisting liver and kidney transplant patients and designed their experiments taking advantage of the naturally occurring difference in mitochondrial DNA between donor and recipient.- Scientists isolated immune cells from transplant recipients
- After three months and six months respectively, the study team exposed the immune cells to mitochondrial protein fragments from the donor as well as recipient
- The immune cells attacked the mitochondrial proteins that were derived from the mitochondrial DNA of the donor only
Sonja Schrepfer, MD, PhD, professor of surgery and senior author of the study, said: "In both mouse and human, even one mitochondrial mutation is enough to have a recognizable immune response."
Mitochondrial Mutations During Conversion of Patient Cells to iPSCs
The conversion process is believed to be capable of causing mutations (mutagenic), especially in the mitochondrial genes due to the following reasons:- Even in normal cells, mitochondrial DNA is 10-20 times more susceptible to mutation compared to nuclear DNA. During the conversion process, the rate is even higher
- Unlike nuclear DNA, mitochondrial DNA does not have cellular mechanisms that recognize mutations and correct them
- Induced pluripotent cells are created in the lab in a petri dish where there are no immune cells. The longer these stem cells stay in the culture medium, the greater the chances of mutation, and increased risk of rejection when transplanted
Can the Rejection of iPSCs Be Prevented?
The authors of this study have earlier discovered a method to make induced pluripotent stem cells (iPSCs) "invisible" to the immune system, an achievement that ensures that patient stem cells differing in mitochondrial DNA are not recognized as foreign and attacked. However, until further research, physicians and research scientists should be aware of the possibility of immune rejection of stem cells differing in mitochondrial DNA and carefully screen for mitochondrial mutations before giving stem cell therapies.In summary, mitochondrial mutations can result in rejection of patient-derived stem cells and it is important to screen stem cells for mitochondrial mutations before introducing into patients to avoid the risk of rejection.
Reference:
- De novo mutations in mitochondrial DNA of iPSCs produce immunogenic neoepitopes in mice and humans, Nature Biotechnology (2019). DOI: 10.1038/s41587-019-0227-7
Source-Medindia