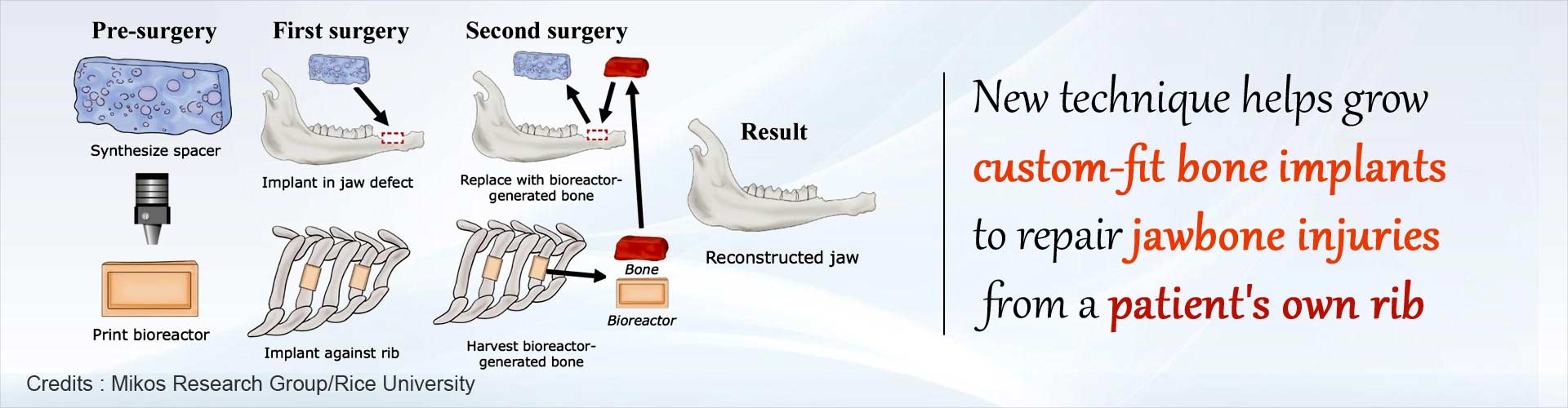
Natural bone made inside the patient by attaching a 3D printed scaffold to patient’s rib can be successfully used as an implant to replace damaged jaw bone in craniofacial reconstruction surgery.
Highlights:
- Natural and strong bone implants to improve outcomes in craniofacial reconstruction surgery can be grown within the patient by attaching a 3D printed scaffold to the patient’s own rib
- Craniofacial injuries are common in battlefield injuries and reconstruction of damaged bone is a complex and long drawn out process
- Current methods of obtaining new bone for implant involve harvesting bone grafts from patient’s hip, leg or shoulder and growing new bone by the addition of external growth factors which requires regulatory approvals and is more complicated
The study was led by bioengineer Antonios Mikos, one of the pioneers in the field of tissue engineering and has culminated in success following a decade-long program sponsored by the Armed Forces Institute of Regenerative Medicine.
The aim of the research was to improve craniofacial surgical reconstruction by using the body’s own natural healing powers
"A major innovation of this work is leveraging a 3D-printed bioreactor to form bone grown in another part of the body while we prime the defect to accept the newly generated tissue," said Mikos, the Louis Calder Professor of Bioengineering and Chemical and Biomolecular Engineering at Rice and a member of the National Academy of Engineering and National Academy of Medicine.
Read More..
How This Study Is Superior To Previous Research
- Previous research demonstrated a technique to produce bone grafts from real bone implanted into the chest cavity.
- In contrast, the current study showed that viable bone grafts could be created from artificial bone substitute materials to create the 3D printed scaffold and a spacer (see below) both namely made of synthetic material termed PMMA (polymethyl methacrylate) or bone cement.
- The spacer mold is placed at the site of craniofacial injury and promotes healing and prevents scar tissue from filling the defect at the site of injury, while the bone implant was being made on the patient’s rib
Creating Natural Bone Implant Using Patient’s Rib
To test their theory, the study team used sheep as the animal model in which a rectangular defect was created in its jaw bone.- The team excised enough bone from the animal’s rib so that the periosteum was exposed. This periosteum would serve as the source of stem cells and blood vessels to seed the attached 3D printed scaffold
- Crushed rib bone or synthetic calcium phosphate materials were used to 3D print the biocompatible scaffold.
- The scaffold, with the rib side open to create a strong attachment point, stayed in place for nine weeks after which the new natural bone was removed and placed in the craniofacial defect replacing the spacer
- In the animal models studied, the new bone wove seamlessly into the bony defect in the jaw and soft tissue grew around this and covered the defect
Why Were Ribs Chosen and Why Was PMMA Chosen as Scaffold and Spacer Material?
- Ribs are a rich source of stem cells
- Since it is made within the patient, it will match the patient’s tissue
- Also, since it is natural bone and does not involve any external factors, elaborate permissions and approvals are avoided
- Multiple bone implants can be made simultaneously using patient’s multiple ribs
Summary
Natural bone implant made in the patient’s own body by attaching a biocompatible 3D printed scaffold to the patient’s rib can be used to improve outcomes in craniofacial reconstruction surgery.Reference:
- Biomaterials-aided mandibular reconstruction using in vivo bioreactors - (https://www.pnas.org/content/early/2019/03/12/1819246116)
Source-Medindia