Combating cervical cancer in India through awareness, affordable screening, and accessible treatments. Time for change is now!
- Cervical cancer is the second most common cancer in Indian women, contributing to 18% of all cases
- Lack of awareness and screening drives high morbidity; early detection is crucial for effective treatment
- Peripheral health workers equipped with VIA and VILI offer cost-effective solutions for rural areas
The Silent Crisis: Cervical Cancer's Toll on Indian Women
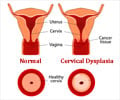
The primary cause of cervical cancer is persistent Human Papillomavirus (HPV) infection, with additional risk factors including early marriage, multiple sexual partners, numerous pregnancies, poor genital hygiene, malnutrition, smoking, immunosuppression (including HIV infection), prolonged use of oral contraceptives, and a lack of awareness and screening. Recognizing warning signs such as irregular vaginal bleeding, bleeding between periods or after sexual intercourse, postmenopausal bleeding, foul-smelling vaginal discharge, lower back pain, or lower abdominal pain is crucial for early intervention.Innovative Solutions: VIA and VILI in Rural Healthcare
Cervical screening methods, such as Pap Smear and HPV tests, are essential but face challenges in availability, especially in remote and rural areas. Dr. Kumar suggests alternative screening methods like Visual Inspection with Acetic Acid (VIA) and Visual Inspection with Lugol's Iodine (VILI), which use substances like acetic acid and Lugol's iodine to detect changes in the cervix visible to the naked eye. These methods can be administered by peripheral health workers, offering a viable solution for regions lacking access to conventional screening tests.Recognizing the financial barriers to Pap Smear and HPV tests, Dr. Kumar advocates for the training of peripheral health workers in VIA and VILI procedures. This approach ensures that abnormalities in the cervix can be identified, and women with positive findings can be referred to gynecologists for further assessment. Women with normal results can benefit from regular screening and surveillance conducted by trained health workers, providing a cost-effective and accessible solution.
To tackle the cervical cancer crisis comprehensively, it is imperative to bridge the screening gap and prioritize HPV vaccination for young girls, despite it is not being part of India's Universal Immunization Program. Additionally, addressing treatment availability challenges, especially in remote areas, is essential for effective prevention and management.
Why Should Boys Also Get HPV Vaccination?
Vaccinating both girls and boys is a crucial step in preventing cervical cancer, according to Dr. Stephanie Ricci, a staff physician specializing in gynecology oncology at the Oncology Institute, Cleveland Clinic Abu Dhabi.Cervical cancer, the fourth most common cancer in women globally, is mainly caused by the human papillomavirus (HPV), a sexually transmitted infection. Dr. Stephanie emphasizes that individuals with multiple strains of HPV are at a higher risk for cervical cancer, especially those with compromised immune systems due to factors such as immunosuppressant medication, obesity, diabetes, and high stress levels.
The HPV vaccine, covering nine high-risk strains, is highly effective in preventing cervical cancer, with strains HPV 16 and 18 accounting for about 70% of cases. Dr. Stephanie advocates for both girls and boys to receive the vaccine, as males can transmit HPV to females, and the vaccine also protects against genital warts. Regular screenings, including pap smears and HPV tests, are vital for early detection and prevention. The Abu Dhabi Public Health Center recommends specific screening intervals for different age groups, emphasizing the importance of lifestyle factors in reducing cervical cancer risk.
In conclusion, cervical cancer is a preventable disease, and urgent steps are needed to enhance awareness, improve screening infrastructure, and ensure widespread access to both preventive measures and treatments. By addressing these challenges, India can make significant strides in reducing the incidence and mortality rates associated with cervical cancer.
"By bridging the screening gap, prioritizing vaccination, and ensuring treatment accessibility, we can pave the way to a cervical cancer-free India."
Reference:
- Cervical Cancer - (https://pubmed.ncbi.nlm.nih.gov/28613745/)
Source-Medindia