A study revealed the prevalence of metabolically healthy phenotype in an aging, obese population but failed to find a link between traditional risk factors and subclinical cardiovascular disease.
There is an undisputed link between obesity and metabolic syndrome (MetS) which is a cluster of conditions including high blood pressure, higher-than-normal blood sugar level, excessive abdominal fat and abnormal cholesterol levels. When these conditions occur together in individuals, it increases a person’s risk of heart disease, stroke and diabetes. Among the obese, the group of individuals who do not suffer from Metabolic syndrome (MetS) are known as “metabolically healthy obese” (MHO).
A cross-sectional study was conducted at the Biocardios Institute of Cardiology, Brasilia, Brazil. In this study, the association of MHO phenotype among those above 80 years with CVD and inflammation was examined. The subjects had to be above the age of 80 years with no clinical evidence of CVD. The study included 208 individuals of 80 years or older, of which 79% were female.
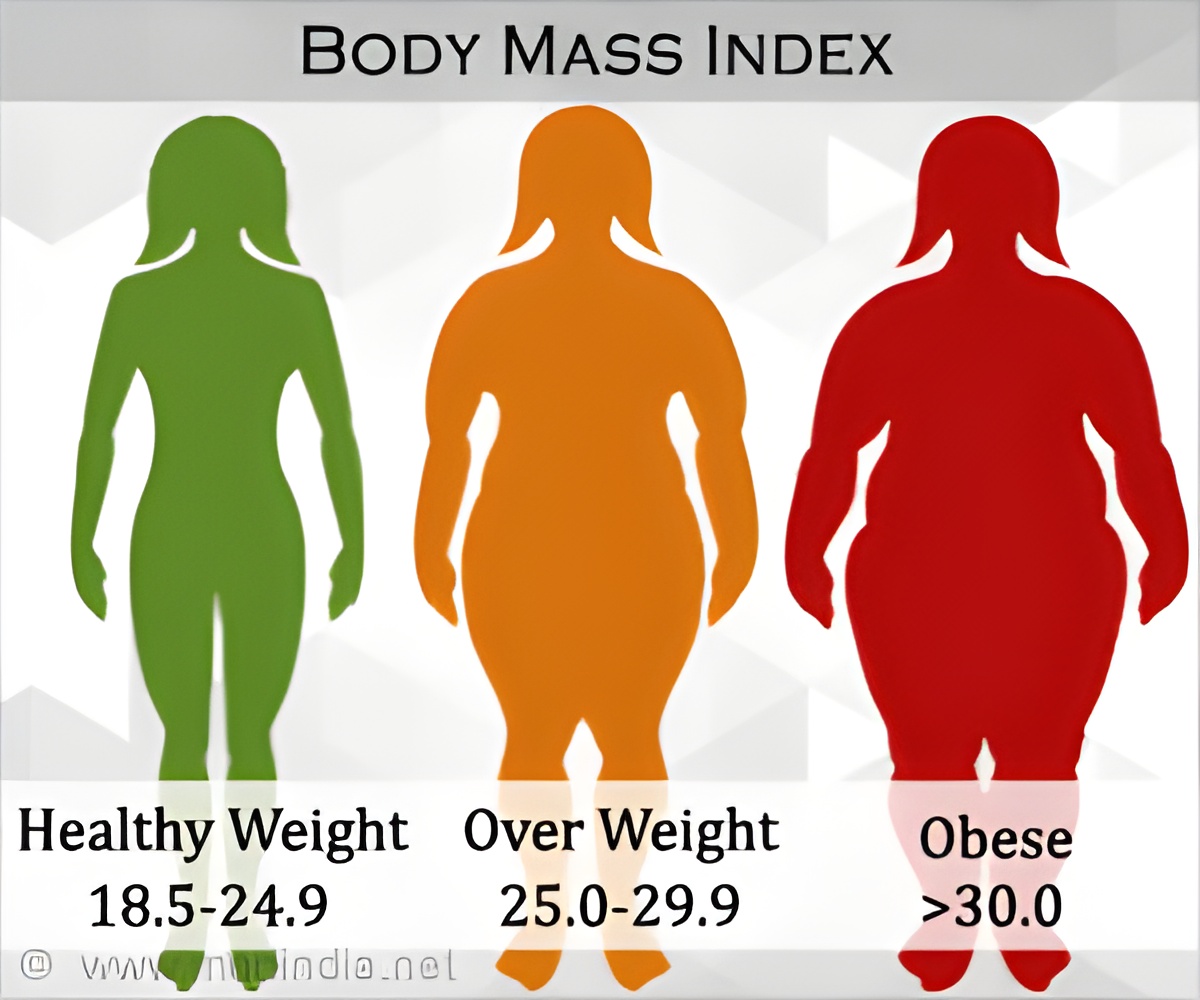
The study population was categorized into four groups - metabolically healthy, normal weight (MHNW); metabolically unhealthy, normal weight (MUNW); MHO (metabolically healthy obese) and metabolically unhealthy obese/overweight (MUHO). Of those studied, 9.0% of men and 14.6% of women were MHO.
For each of these patients, the BMI was calculated and the subjects were categorized into:
- Normal weight - BMI< 25
- Overweight /Obese -BMI equal to or > 25
- >88 cm – women
- >102 cm for men.
- Moderate-intensity aerobic activity for 150 minutes per week
- Vigorous-intensity aerobic physical activity for 75 minutes per week
- An equivalent combination of both the above mentioned activities
- Systolic blood pressure (systolic ≥130 mmHg) and diastolic blood pressure (≥85 mmHg )
- Fasting blood glucose (FBG) ≥110 mg/dL / or individual on diabetes medication
- HDL-C <50 mg/dL in women, <40 mg/dL in men or if the patient was on nicotinic acid
- Triglycerides ≥150 mg/dL or the patient was on fibrates
The coronary artery calcium score (CACS) was determined using cardiac CT. If it was equal to 0, then the individual was normal and had no symptoms of subclinical atherosclerosis (CVD).
Relationship between Obesity and Cardio Vascular Disease (CVD)
Obesity is directly linked to cardiovascular diseases (CVD), Type-2 diabetes and hypertension Tot; and all these conditions are characterized by resistance to insulin-mediated glucose disposal (insulin resistance). Not all obese individuals are insulin resistant; however, almost all insulin–resistant individuals tend to be obese. Insulin resistance in obese individuals can be reversed through weight loss yet, not many physicians are into weight-loss counseling and the health care system, too, is not equipped to deal with the consequent disease burden.In accordance to the results of the study, the usefulness of traditional risk factors, such as hypertension, need to be re-considered while evaluating the elderly population for the risk of cardiovascular disease. The majority of them have at least one risk factor but what was interesting was that about 11.9% of those studied had a calcium score of CACS = 0 which make them low risk for CVD. This shows that the presence of traditional risk factors alone are not enough to classify this population based on risk. It is suggested that the extent of subclinical CVD be assessed carefully in order to understand disease progression in this group.
The world has agreed on the fact that it is in the midst of an obesity epidemic. However, public awareness is still wanting when it comes to dealing with issues at hand.
References:
1. The prevalence of the metabolically healthy obese phenotype in an aging population and its association with subclinical cardiovascular disease: The Brazilian study on healthy agingLara Roberson1, Sameer Shaharyar2, Ehimen Aneni1, Wladimir Freitas3, Michael Blaha4, Arthur Agatston1, Roger Blumenthal4, Raul D Santos5, Hamid Feiz2, Khurram Nasir1678* and Andrei Sposito9
Diabetology & Metabolic Syndrome 2014, 6:121
2. http://www.ncbi.nlm.nih.gov/pubmed/21855697
Source-Medindia