Obesity surgery has proven to be just as effective for teenagers as for adults with gall stone formation and micronutrient deficiency as side effects.

- Gastric bypass surgery in obese teenagers were as effective as that in adults.
- Bowel obstruction and gall stones were the common side effects after the surgery.
- Long-term monitoring after bariatric surgery is necessary for better management.
For the study, 81 teenagers underwent gastric bypass surgery. There were two comparison groups; a similarly large group of young people receiving traditional treatment, and also a group of adults undergoing gastric bypass. Sixty-five percent were female and 35 percent were male.
The young people who had the surgery were between 13 and 18 years old at the time of the procedure, with an average age of around 16 and having an average BMI of around 45 kg/m2. In many cases, their obesity had already led to complications, such as disturbed blood lipids, high blood pressure, fatty liver disease, type 2 diabetes or the early stages of diabetes.
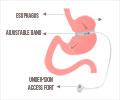
The surgery, a keyhole procedure in which the small intestine is connected to a small stomach pouch just below the esophagus, takes roughly one hour to complete. The main part of the stomach remains in place and produces gastric juices which, together with bile, enter the system further downstream. In principle, this means that the food goes directly into the small intestine.
"We're talking about the young people having the severest obesity. Without surgery, they will, with almost no exceptions, remain big for the rest of their lives. In teenagers it is obvious that there is a strong underlying genetic predisposition for developing severe obesity -- it is not a lifestyle choice by any means," says Torsten Olbers.
One in four of the teenagers who had had the surgery did, however, experience complications and required further surgery within five years, for either bowel obstruction (in about half the cases) or gallstones (the other half).
After a gastric bypass, there is a risk that patients develop deficiencies of vitamins and minerals due to the reduced food intake and also due to the new arrangement of the digestive system. This was also evident in young people in the study, who often were reluctant to take the recommended supplements.
"It is very important that we continue to monitor these young people, especially given that they have many decades of living left to do," Torsten Olbers adds.
The patients in the study were monitored at several centers across the country as part of a process which involved researchers from both Lund University and Karolinska Institute, where Claude Marcus is a professor in Pediatrics.
Based on the findings, young people who undergo bariatric surgery need a lot of support to manage their life after surgery.
Reference
- Torsten Olbers et al., Positive outcomes after obesity surgery in adolescents, The Lancet Diabetes & Endocrinology (2017) http://www.thelancet.com/journals/landia/article/PIIS2213-8587(16)30424-7/fulltext.
Source-Medindia