Research highlights a connection between belly fat and chronic musculoskeletal pain. Reducing abdominal fat may offer relief, especially in women, who are twice as affected.

- Excess belly fat is linked to chronic pain affecting multiple body areas
- Women are twice as likely to suffer from multisite chronic pain due to abdominal fat
- Reducing abdominal fat can be a potential strategy for managing chronic pain
MRI-derived abdominal adipose tissue is associated with multisite and widespread chronic pain
Go to source).
Reducing abdominal fat can alleviate widespread musculoskeletal pain, particularly in women. #medindia #chronicpain’
A Global Epidemic of Musculoskeletal Pain
Musculoskeletal pain, which affects bones, joints, ligaments, tendons, and muscles, is a global health problem. Approximately 1.71 billion people suffer from some form of this pain worldwide. The condition can be debilitating and persistent, affecting one’s quality of life.Belly Fat and Chronic Pain: The New Link
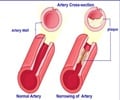
Previous studies have established a connection between obesity and musculoskeletal pain, but the link between excess body fat and chronic pain affecting multiple body parts has remained unclear. Researchers from the University of Tasmania and Monash University in Australia set out to explore this connection, focusing on the impact of abdominal fat on chronic pain.The study found that abdominal fat—both the fat surrounding internal organs (visceral adipose tissue or VAT) and fat just beneath the skin (subcutaneous adipose tissue or SAT)—is linked to chronic musculoskeletal pain. The researchers concluded that excess fat, particularly in the abdominal region, may play a role in the development of chronic, multisite pain.
“Abdominal adipose tissue was associated with chronic musculoskeletal pain, suggesting that excessive and ectopic fat depositions may be involved in the pathogenesis of multisite and widespread chronic musculoskeletal pain,” the study noted.
Implications for Chronic Pain Management
The study involved 32,409 participants, half of whom were women, with an average age of 55. All participants underwent MRI scans to measure their levels of visceral and subcutaneous fat. Over 600 participants were reassessed after two years to observe changes in their pain levels and body fat distribution.The results showed a significant link between chronic pain and the amount of visceral and subcutaneous fat, as well as body mass index (BMI). Women were found to be twice as likely to suffer from multisite chronic pain as men, with sex differences in fat distribution and hormone levels likely contributing to the discrepancy.
The findings of the study suggest that targeting abdominal fat loss could be a new avenue for managing chronic pain. Reducing abdominal adiposity may not only improve overall health but also alleviate the burden of chronic pain, particularly for those experiencing pain at multiple body.
As chronic pain continues to affect millions worldwide, this research offers a potential solution for those seeking relief from their symptoms. By focusing on reducing belly fat, individuals may improve their quality of life and experience less pain over time.
Chronic pain is a complex and challenging condition, but this new research sheds light on the role of abdominal fat in its development. By taking steps to reduce belly fat, individuals may find relief from persistent musculoskeletal pain, especially women who are disproportionately affected.
Reference:
- MRI-derived abdominal adipose tissue is associated with multisite and widespread chronic pain - (https://rapm.bmj.com/content/early/2024/08/06/rapm-2024-105535)
Source-Medindia