Anti-parasitics are a class of drugs that are indicated for the treatment of parasitic diseases such as cestodes, nematodes, trematodes, amoebas and infectious protozoa.
The parasitic infections can result in fetal or neonatal damage, cutaneous nodules, (a small mass of tissue or aggregation of cells found on the skin), nutritional deficiencies, skin eruptions, as well as major damage to eyes, lungs, heart, central nervous system or liver.
Infections such as schistosomiasis, leishmaniasis, amebiasis and trypanosomiasis are the pioneer causes of mortality around the globe.
Joel Thome and Mary Wen, both from the Washington State University College of Pharmacy, Washington, reviewed literature on the prevalence of drug therapy for parasitic infections in the United States. It was published in US Pharmacist 2012.
Owing to better living, water, and food standards, people in the United States are less affected by the parasitic infections. United States is naturally blessed with protective climate particularly in the northern region. The citizens of America are chiefly affected when traveling to the tropical regions, or when in direct contact with immigrants or people newly immigrated to the U.S. Rarely the infection is caused by direct contact with animals or pets and improperly cooked food.
Drug therapy and prevention methods for common parasitic infections in the U.S. is described here.
This group of drugs is chiefly used for treating and preventing malaria. The travelers are advised to take two doses before entering malaria-endemic region and then continue for four weeks after returning back.
The patients should be educated about the importance of prevention of the bite of Anopheles mosquito.
Effective prevention can be achieved by wearing long-sleeved and long-legged clothing, using mosquito nets and applying strong insect repellants.
Drugs such as hydroxychloroquine and amodiaquine are rarely employed for monotherapy. However they are sometimes used against chloroquine-resistant strains.
Metronidazole and Tinidazole:
Metronidazole and tinidazole are the best available choice of treatment against amebiasis, giardiasis and trichomoniasis. ‘Drug therapy for amebiasis should generally consist of a luminal agent that is capable of eradicating the luminal (intestinal) infection’ say the authors.
The recommended dose of metronidazole is 750mg orally three times a day or 500mg intravenously every 6 hours for 10 days.
Metronidazole combined with chloroquine is effective for treating hepatic abcess or extraintestinal disease.
Metronidazole in the doses of 250mg three times a day with meals for five days is effective in curing giardiasis. A single dose of 2g tinidazole also gives useful results. Other options are nitazoxanide or paromomycin.
Metronidazole in the single dose of 2g can treat trichomoniasis. Dyspepsia may be present with this therapy so metronidazole 500mg twice daily can be given for seven days. Although, less effective, tinidazole can also be given instead of metronidazole.
‘Intravaginal metronidazole is intended for bacterial vaginosis, and not Trichomonas vaginalis’ caution the authors.
Metronidazole is associated with nausea, dermatologic reactions, vaginal candida infection and parageusia (bad taste in the mouth). Certain neurologic reactions such as headache, dizziness, peripheral neuropathy, disorders of special senses (optic or auditory nerve disorders), seizures, etc. are also seen.
Other side effects associated with metronidazole are aseptic meningitis, leucopenia, hemolytic uremic syndrome and encephalopathy.
Alcohol should be avoided during this drug therapy so as not to risk a disulfiram-like reaction.
Ivermectin:
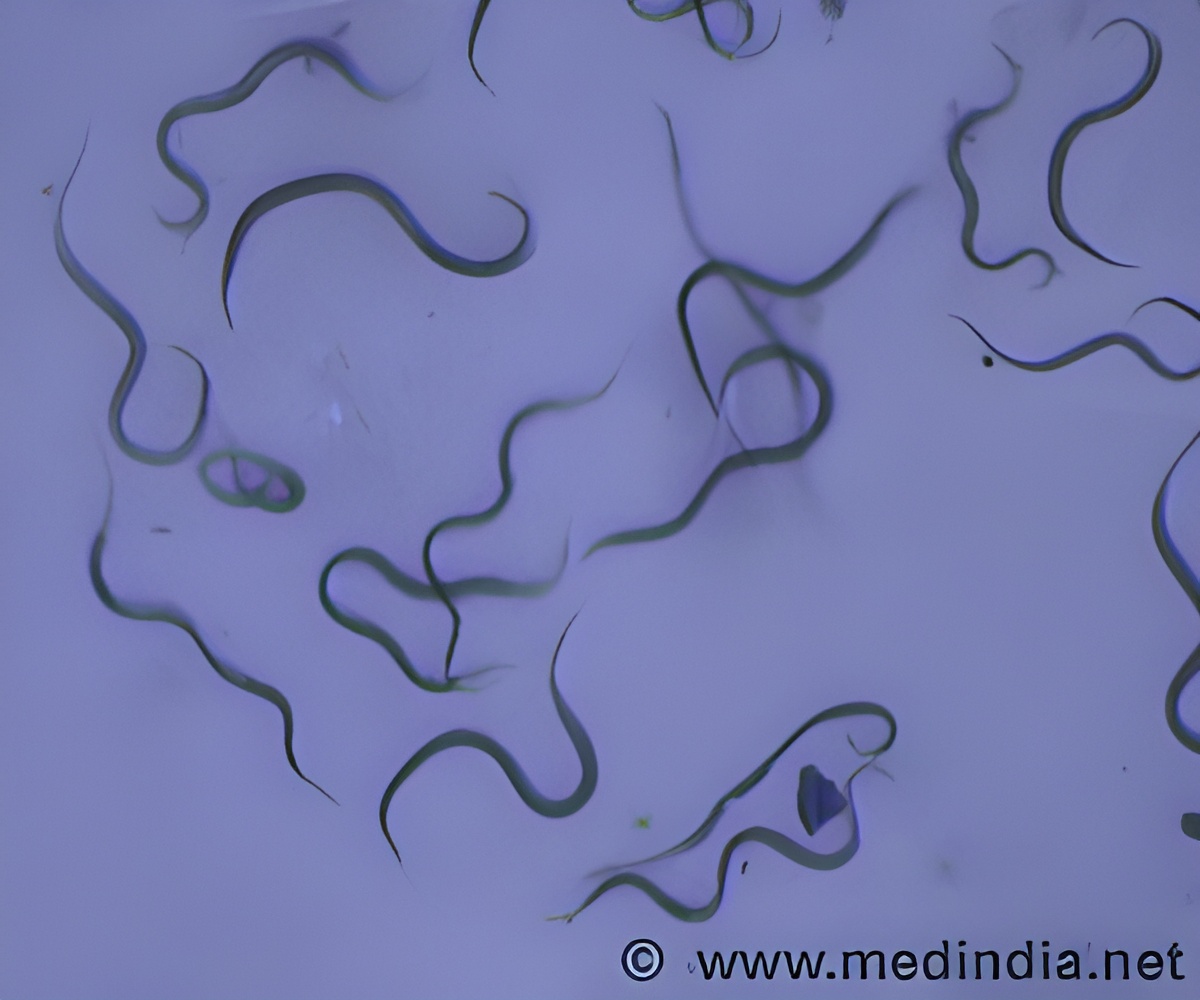
Ivermectin is the most popular antiparasitic but not the most effective drug in the United States. Although it is FDA approved for systemic infections by larval forms of Onchocerca volvulus and intestinal strongyloidiasis (infected by small intestine roundworms), but it is widely used for lice, scabies and enterobiasis (pinworms).
In southern Mexico and Guatemala, ivermectin is extensively used for eradicating onchocerciasis (a disease caused by black flies depositing larvae of Onchocerca volvulus under the skin).
Ivermectin works by inactivating certain helminths (roundworms and tapeworms) through hyperpolarizing their neurons ((making the parasite neurons more negatively charged).
Ivermectin is normally given as a single dose. Repeat doses might be required once or twice a year.
Side effects of ivermectin include dizziness, fatigue, rash or abdominal pain. Other associated effects can be lymphangitis, peripheral edema, myalgias, hypotension, arthralgias, tachycardia and lymphadenitis.
Pyrantel Pamoate:
Pyrantel pamoate is used for curing enterobiasis, usually caused by pinworms (Enterobius vermicularis). Pyrantel pamoate is also used against ascariasis and is employed as an alternative for mebendazole for hookworms.
Common adverse effects of pyrantel pamoate are dizziness, somnolence and headache.
Albendazole:
Albendazole is FDA approved and as effective as mebendazole against helminth infestation. It is highly effective in treating neurocysticercosis (tapeworm larvae invading the central nervous system of humans) and echinococcosis (allergic reactions and damage to organs by larva of tapeworm; infecting humans through contact with dogs and livestock).
‘For luminal infections (e.g., ascariasis), the dose can be given on an empty stomach to reduce absorption. For systemic or extraintestinal infections, albendazole can be given with food to enhance absorption’ recommend the authors.
Prolonged therapy of albendazole is associated with deleterious side effects.
Adverse Effects of Antihelminthic Drugs:
The adverse effects of antihelminthic drugs depend upon the duration of treatment. Some adverse effects may occur when the parastic worms are dying rather than when they directly infect humans.
Special Considerations When Treating Ocular or CNS Infections:
In the U.S. about 66 percent patients have seizures and are on antiseizure therapy. Globally neurocysticercosis is the primary cause of symptomatic seizures.
‘The use of a glucocorticoid (e.g., prednisone) can greatly reduce morbidity when treating certain CNS (central nervous system) manifestations of parasitic infections, particularly certain forms of neurocysticercosis—cysticercal encephalitis, subarachnoid neurocysticercosis, and spinal intramedullary cysticercosis.’
Combining a glucocorticoid with albendazole may reduce damaging inflammation at the site of infectio, suggest the researchers.
An important point to keep in mind is that ‘Antiparasitic drug therapy is not always indicated for CNS or intraocular infections because dying helminths may cause more damage than live ones.’
Praziquantel should not be used while treating ocular infections particularly with dexamethasone. In case of CNS or eye infection, a neurologist or an ophthalmologist should be consulted before the onset of the treatment.
Availability of Antiparasitic Drugs :
Most of the harmful agents for curing parasitic infections are not used in the United States because of low occurrence of infections.
Drugs not approved for use in the U.S., may in some cases be procured from the CDC if it is on the Investigational New Drug (IND) list with the FDA.
Reference:
1. Drug Therapy for Common Parasitic Infections Within the United States; Joel Thome et al; US Pharmacist 2012
Source-Medindia








