Teenager with sickle cell disease achieved complete remission after an experimental gene therapy.
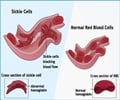
- Sickle cell anemia which is an inherited blood disorder causes the aggregation of sickle-shaped red blood cells in the blood vessels, blocking blood flow.
- Previous treatments for sickle cell anemia like hematopoietic stem cell transplant, required a patient’s bone marrow to be replaced with outside donors.
- In gene therapy, the patient’s bone marrow was removed and genetically altered to compensate for the defect in the DNA responsible for sickle cell disease.
Before the commencement of the treatment, the teenager had to visit the hospital monthly for blood transfusion and excessive amount of treatment had caused severe internal damage. The 13 year old already needed a hip replacement and had his spleen removed.
“Since therapy was applied, he hasn’t had any pain, any complications. He is free of any transfusions. He plays sports and goes to school,” said Dr. Philippe Leboulch, an author of the new research and a professor of medicine at the University of Paris. “So we are quite pleased with the results.”
Doctors at Necker Children’s Hospital removed the teenager’s bone marrow and genetically altered it using a virus to compensate for the defect in his DNA responsible for sickle cell disease.
Dr. Marina Cavazzana, senior author of the study and head of the biotherapy department at Necker, said, “all the biological tests we perform lead us to think he is cured.” Yet, she added, the answer to the question of whether he is truly cured “can be provided only by the longer follow-up.”
Sickle cell disease is a severe hereditary form of anemia in which people have abnormal hemoglobin due to genetic mutation in their red blood cells.
More than 275,000 infants are born with sickle cell disease annually, worldwide.
In the United States, approximately 100,000 people, currently have the condition. Most of them are of African ancestry. About one in every 365 black children in the US is born with sickle cell disease. The life expectancy for sickle cell is now about 40 to 60 years.
According to the US Centres for Disease Control and Prevention, sickle cell trait is common among people who live in areas where malaria is endemic.
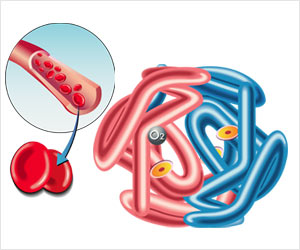
Sickle cell disease increases risk of other serious infections or anemic, as the red blood cells cannot carry enough oxygen around the body. This can cause tiredness and shortness of breath.
Regular blood transfusions, every three to four weeks, are required in some cases.
Procedure
In the new therapy, researchers tried to inhibit the process of aggregation of the distorted red blood cells.
The researchers harvested the stem cells from the patient’s own bone marrow and altered the genetic instructions so that they would make normal hemoglobin.
Then, they treated the patient with chemotherapy for four days to eliminate his diseased stem cells.
Finally, they returned the treated stem cells via an IV into the bloodstream of the patient.
“At that point, the new cells that were modified outside the body started to make new blood cells, and we hope this will be stable for the life of the patient,” Leboulch said.
Benefits of Gene Therapy
Gene therapy is easier on patients than procedures that require outside donors like hematopoietic stem cell transplant, which replaces a patient’s bone marrow with that of a donor.
Though hematopoietic stem cell transplant has proven to be an effective cure for some patients, majority of sickle cell disease patients do not have a sibling who would be an appropriate match for bone marrow donation.
According to Dr. Alexis Thompson, president-elect of the American Society of Hematology, “Gene therapy holds promise because a patient serves as his own donor,” and the “risks are much reduced” since there’s no possibility of a mismatch.
“I think this is a really very exciting advancement,” she said, adding that if the results seen in France can be duplicated, this would provide “for a new direction for patients who need a curative option.”
Future
The future plan is to proceed to clinical trials and if results are promising, make the treatment available to patients.
Researchers are using the same genetic therapy to treat a similar disease called thalassemia, another inherited blood disorder in which patients have less hemoglobin and fewer red blood cells than normal. Severe forms require regular blood transfusions.
“I understand that seven (sickle cell) patients have been treated already. Of course, the outcome is much shorter, and we don’t have the results just yet, but it’s coming along,” Leboulch said. “To apply this to a baby or a very young child should be at least as effective or more,” he said. “Doing it with older patients, who have had years of complications, could be more challenging.”
“Now, we want to be cautious, of course, and we don’t want to say that this is the cure for tomorrow or the next day for everybody,” Leboulch said. “At the same time, what we’ve observed is really convincing, and we just hope that we can move this along to make it available to patients.”
The findings are published in The New England Journal of Medicine.
Reference
- Marina Cavazzana et al. Gene Therapy in a Patient with Sickle Cell Disease. The New England Journal of Medicine.; (2017) DOI: 10.1056/NEJMoa1609677
Source-Medindia